Proven medical techniques for managing testicular pain and fostering recovery
Whether resulting from injury, infection, or an STI, testicular pain and swelling can be highly discomforting. The most effective approach to alleviating your discomfort typically depends on the underlying cause, yet there are established remedies you can employ independently at home. Continue reading to discover optimal strategies for diminishing pain and swelling, along with methods for addressing common sources of testicular discomfort.
Essential Information
- Apply an ice pack to alleviate pain and diminish swelling in your testicles.
- Recline on your back and position a folded towel beneath your testicles for enhanced comfort.
- Utilize supportive underwear or a jockstrap to alleviate discomfort.
- Follow your doctor's prescription for antibiotics to combat bacterial or sexually transmitted infections causing testicular pain and swelling.
Procedure
Seeking Rapid Relief

Utilize an ice pack on the affected area. In cases of sudden swelling and pain, gently apply an ice pack or a makeshift one using ice cubes and a plastic bag. If an ice pack is unavailable, create one at home.
- If the swelling is severe, applying an ice pack can prolong the viability of the testicles without adequate blood supply.
- Wrap the ice pack or frozen vegetables in a dry cloth before application to prevent frostbite.

Recline on your back. Until professional medical assistance is accessible, lying down and supporting the testes can alleviate physical strain and discomfort. Find a comfortable position that reduces pain levels.
- Support your testicles by placing a rolled-up towel underneath for pain relief.

Take a soothing warm bath. Immersing yourself in a warm bath can alleviate some discomfort. Take baths as necessary to experience relief.

Opt for a jock strap or supportive undergarments. Additional support may alleviate pain. If comfortable, wear a jock strap or supportive underwear until pain and swelling subside.

Utilize over-the-counter pain relievers. Ibuprofen, paracetamol, or aspirin can effectively alleviate pain and swelling. These medications work by inhibiting prostaglandin production, reducing inflammation. Recommended dosages are as follows:
- Ibuprofen (or similar generic drug), 200 – 400 mg tablets, with or just after food, up to 3 times a day
- Aspirin, 300 mg tablets up to 4 times a day
- Paracetamol, 500 mg tablets up to three times a day
- Avoid mixing these medications as overdose can result in serious side effects.
Rest and avoid strenuous activities. Allow the testicles to heal naturally by refraining from activities that could exacerbate pain and swelling. Avoid heavy lifting, running, and other vigorous exercises.
- If prolonged rest isn't feasible, wear supportive underwear to help alleviate pain.
Common Causes of Testicular Pain or Swelling

Trauma Testicular trauma, known as testicular torsion, entails pain in the testicles and epididymis, the tube beneath the testicles. Any testicular trauma, particularly torsion, warrants professional attention as it may pose a threat to the testicle's well-being.
- Your doctor may assess your Cremasteric reflex, absent in trauma cases. They'll test this by using a reflex hammer along the inner thigh, causing the testicle to rise into the scrotal sac in healthy cases.
- Testicular torsion typically manifests as sudden pain.

Infection Infectious causes of testicular pain include bacterial infection of the testicles and epididymis. Bacteria often migrate from the rectum, particularly in men older than 35 and younger than 14. In younger men aged 15 to 35, sexually transmitted bacteria like chlamydia and gonorrhea are common culprits. Elevated testicles may alleviate pain, known as Prehn’s sign.
- Identify chlamydia symptoms and recognize gonorrhea symptoms such as painful urination or penile discharge.
- Treating the infection helps alleviate pain and prevents its worsening, potentially leading to sepsis.
- The Cremasteric reflex persists despite pain from infections.

Orchitis Orchitis results from a viral infection, causing sudden pain and swelling in the testicle. It often arises from mumps orchitis, a viral infection linked to mumps. Around 20 to 30% of children with mumps develop mumps orchitis, typically occurring a week after parotitis onset, characterized by swelling of the parotid glands below the jaw.
- No specific treatment exists for viral mumps orchitis, potentially leading to infertility. Supportive care like pain relief and ice packs is crucial.

Sexually transmitted infections (STIs) Identify STI symptoms such as testicular pain and discomfort during urination. Symptoms typically manifest gradually over weeks, accompanied by vomiting, nausea, or abdominal pain. Cremasteric reflex remains unaffected.
- Ultrasound may reveal heightened vascularity, pockets of infection, or abscesses.
- Other symptoms may include discharge or blood in the urine.

Epididymo-orchitis Rapid onset of pain due to bacterial infection leads to swelling and enlargement of the epididymis and testicles, which become tender, red, and painful.
- Additional infections like urinary tract infections or urethral infections may also occur.

Hypogonadism Hypogonadism occurs when the body fails to produce sufficient testosterone or sperm. It can be congenital or acquired due to injury, resulting in painful, swollen genitals, erectile dysfunction, and infertility.
- Pituitary disorders, inflammatory diseases, and certain medications can also trigger hypogonadism.
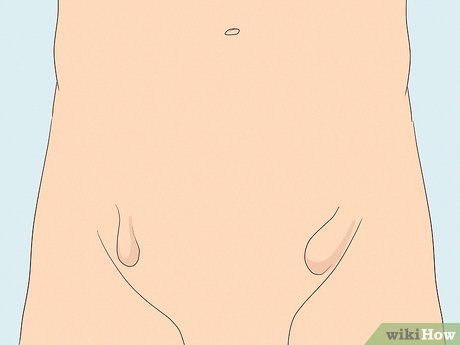
Hernia Hernias develop when tissue protrudes through a muscle into another body part. Inguinal hernias, common among AMAB individuals, occur when abdominal tissue bulges into the groin, leading to testicular pain and swelling.
- Hernias are prevalent, often resulting from strenuous activity or injury.
Addressing Common Causes

Undergo lab tests to detect infections. Your physician may examine your urine for bacteria or look for signs of E. coli infection. For sexually active young men, a urine multiplex polymerase chain reaction (M-PCR) can detect chlamydia or gonorrhea.
- An ultrasound is typically conducted for all cases of scrotal pain and swelling to rule out more complex issues.
- Your physician may also check for a hydrocele, a buildup of fluid around the testes. If present, fluid drainage may be performed in-office. However, due to recurrence risk, surgery may be recommended if the hydrocele causes significant discomfort.

Use antibiotics for bacterial infections. Infections causing testicular pain can affect men of any age and may be triggered by E. coli or other bacteria. In older men, benign prostatic enlargement can contribute to these infections by obstructing bladder drainage, allowing bacterial accumulation.
- Treatment typically involves Bactrim DS or a quinolone antibiotic for about 10 days, unless prostate involvement necessitates longer therapy.
- Pain relief options include Tylenol, Motrin, or stronger narcotic pain medication initially.

Treat sexually transmitted infections with antibiotics. Your physician may prescribe Rocephin followed by Zithromax or doxycycline. Pain relief may begin within 24 to 48 hours. Utilizing ice packs and elevating the testicles can provide comfort while awaiting antibiotic efficacy. Over-the-counter pain medications can also be beneficial, especially initially.

Promptly treat infections to prevent long-term complications. Several common risk factors predispose individuals to bacterial and viral infections causing testicular pain. These factors include:
- Sexual activity
- Vigorous physical activity such as frequent cycling or motorcycle riding
- Prolonged sitting, such as frequent travel or long hours of driving
- History of prostate or urinary tract infections
- Benign prostatic enlargement or prostate surgery, particularly in older men
- Anatomical abnormalities like a posterior urethral meatus, which can occur in prepubescent boys

Undergo surgery for testicular trauma. Testicular trauma arises when a twisted testicle lacks adequate blood flow. This often follows various traumas, such as falls from bicycles resulting in groin injuries. Severe trauma can lead to spermatic cord torsion, necessitating surgical intervention. This condition affects approximately 3.8% of males under 18 per 100,000 annually.
- Early detection of a high-riding testicle and absence of the Cremasteric reflex warrants surgical exploration to prevent orchiectomy, the surgical removal of the testicle.
- Even moderate trauma can induce swelling, tenderness, high fevers, and frequent, urgent urination.
- The timeframe from injury to surgery typically ranges from 4 to 8 hours. Swift action prevents extensive damage to the spermatic cord, which must be swiftly untwisted to avoid removal. Despite prompt intervention, orchiectomy rates average 42%. However, delayed diagnosis may necessitate orchiectomy and potentially lead to infertility.
Guidelines
Precautions
- If you endure severe, persistent pain, seek immediate medical attention as it could indicate testicular torsion, requiring urgent medical intervention.
