Dealing with a sick child who experiences frequent vomiting can be concerning. However, it's important to remember that vomiting is often not a serious issue and can usually be managed at home until symptoms subside. If the problem persists or worsens, seeking medical advice is advisable.
Recommended Actions
Providing Home Remedies

Ensuring Adequate Hydration: Vomiting can lead to significant fluid loss, so it's crucial to keep your child hydrated throughout their illness. Water is the best choice, but offering a variety of clear liquids can help maintain hydration levels.
- Encourage your child to sip liquids slowly and frequently, aiming for a drink every five to 10 minutes if possible. Ensure they have access to a beverage at all times.
- Opt for clear liquids predominantly, although some carbonated drinks like ginger ale or lemonade might provide relief.
- Frozen treats such as ice pops or Italian ices can also contribute to hydration. Choose water-based options rather than ice cream, which may irritate sensitive stomachs.
- Broth-based soups, particularly clear varieties like chicken noodle soup, can be beneficial for hydration.
- Exercise caution with sports drinks, as their high concentration can exacerbate symptoms. Pediatric rehydration fluids or plain water are preferable alternatives.

During active vomiting episodes, refrain from giving your child solid foods for 24 hours. For the initial 24 hours of vomiting, it's best to avoid solid foods and opt for electrolyte solutions recommended by your pediatrician. Instead, offer alternatives like gelatin, sugar water, and popsicles.
- Most children experiencing vomiting won't have an appetite for solid foods.
- Some children might mistakenly interpret stomach cramps as hunger and insist on eating; be cautious if your child tends to do this.

Avoid Strong Odors and Other Nausea Triggers. Certain odors can trigger nausea in children (and individuals in general). Food smells, cooking aromas, perfume, smoke, heat, humidity, and flickering lights can exacerbate nausea. Keep the child in a comfortable, well-lit environment free from strong odors if they're sensitive to smells.

Encourage Rest for the Child. A nauseous child will typically feel lethargic, but some may ignore symptoms when engaged in exciting activities. Although some children may become hyperactive when feeling unwell, excessive physical activity can worsen symptoms.
Consult a Pharmacist Regarding Over-the-Counter Medications. Over-the-counter anti-nausea medications may offer relief, but many aren't suitable for children. Seek advice from a doctor or pharmacist to find a safe option for your child's upset stomach. Follow dosage instructions carefully.

Introduce Bland Foods to Your Child. After 24 hours without vomiting, you can gradually reintroduce solid foods. Opt for bland options with mild taste and texture, which are easier on the stomach.
- The BRAT diet (bananas, rice, applesauce, and toast) was previously recommended by some pediatricians for its easy digestibility. While it lacks sufficient nutrients for healing, it may help alleviate nausea during the initial illness phase. Afterwards, transition to a balanced diet rich in healthy carbohydrates, fruits, and vegetables.
- Consider offering gelatin, crackers, cereal, fruit, and salty or high-protein foods if your child can tolerate them.
- Avoid high-fat and spicy foods, as they can exacerbate symptoms. Wait at least six hours after vomiting before reintroducing solid foods.
When to Seek Medical Attention

Recognizing When Medical Attention is Necessary. While nausea is often caused by mild illnesses like bugs or flu and usually resolves without medical intervention, certain situations warrant a visit to the pediatrician.
- If vomiting persists for more than 24 hours (or 12 hours in infants under one year old), medical attention is advised.
- Babies and young children are more susceptible to dehydration. If signs such as dry mouth, absence of tears when crying, weakness, reduced urination, or lethargy are observed, prompt medical evaluation is crucial.
- Promptly seek medical assistance if your child vomits blood or passes bloody stools, as this may indicate a serious medical issue.
- Children with high fever accompanied by vomiting or diarrhea, or experiencing severe abdominal pain, should be seen by a doctor.
- If clear liquids cannot be kept down, medical intervention may be necessary for rehydration or prescription medication for nausea and vomiting. Suspected food-related illnesses should also prompt a visit to rule out food poisoning or other serious conditions.

Schedule a Physical Examination for Your Child. If your child's inability to retain food persists, arrange for a medical evaluation. The doctor will conduct a comprehensive medical history review, physical examination, and may order additional tests such as blood work depending on the symptoms.
Discuss Medication Options with Your Doctor. Your physician may recommend medication to alleviate vomiting. Inquire about dosage and potential side effects for a better understanding.
- Various medications, including anti-nausea, anti-anxiety, and occasionally sedatives, may be prescribed to manage symptoms.
- Preventative therapies may be suggested for children prone to frequent vomiting episodes, aiming to reduce their occurrence.

Explore Stress Management Techniques. If recurrent vomiting is associated with stress, consider stress management strategies to address underlying causes.
- Stress management techniques aim to enhance awareness of early stress signals and often include relaxation exercises like deep breathing. Behavioral strategies may also be taught by a therapist to alleviate stress.
- Consult your doctor for guidance on stress management therapy and potential referrals to therapists, or explore options through your insurance provider.
Consider Nutrition Therapy. Nutrition therapy aims to identify potential food triggers contributing to vomiting episodes. A registered dietitian can collaborate with you and your child to develop customized meal plans addressing their specific dietary requirements. Consult your pediatrician to inquire about nutrition therapy and receive recommendations for a suitable dietitian.
Strategies for Ensuring Hydration and Establishing a Food Reintroduction Plan
 Techniques for Ensuring Proper Hydration in Children
Techniques for Ensuring Proper Hydration in Children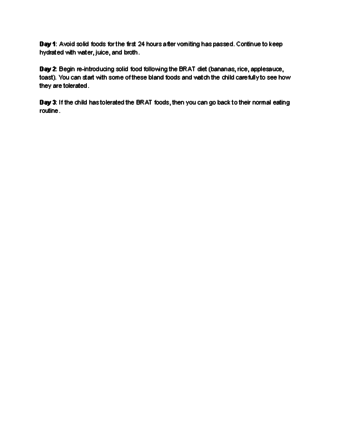 Approach for Gradually Reintroducing Food to Children Following Vomiting Episodes
Approach for Gradually Reintroducing Food to Children Following Vomiting EpisodesUseful Suggestions
-
Promote relaxation with calm activities such as watching a movie, coloring, or reading books.
-
Keep a large plastic bowl beside your child's bed at night to prevent them from rushing to the bathroom if they need to vomit.
-
Place old towels on surfaces like beds and couches to minimize mess in the event of vomiting.
