The ophthalmoscope, also known as a fundoscope, is a medical device utilized to inspect the inner structures of the eye, such as the retina, fovea, choroid, macula, optic disc, and blood vessels. Optometrists and general practitioners employ the ophthalmoscope for diagnosing or monitoring eye diseases, as well as conditions like hypertension and diabetes. Mastering the ophthalmoscope requires proper understanding and ample practice.
Procedures
Prepping Your Device

Ensure the functionality of the ophthalmoscope. Switch it on to check the light. If it doesn't work, replace the batteries and try again. Look through the aperture (eyepiece) for clarity. Remove or open the aperture cover if present.
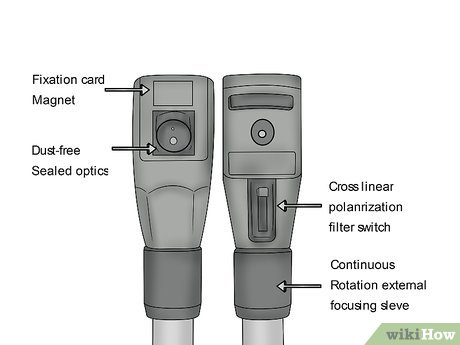
Choose the right setting. There are various aperture and filter options for specific purposes during an eye examination. Typically, the Medium light source is preferred for exams conducted in dimly lit rooms without mydriatic (dilating) eye drops. While ophthalmoscopes may vary in available settings, some common options include:
- Small light – for narrow pupils, such as in bright environments
- Large light – for fully dilated pupils, such as with mydriatic drops
- Half light – for obscured corneas, like with cataracts, to direct light into clear areas of the eye
- Red free light – for enhanced visualization of blood vessels and vascular issues
- Slit – for detecting contour irregularities
- Blue light – for post-fluorescein staining to identify abrasions
- Grid – for measuring distances

Adjust the focus using the focusing wheel. Typically, set your ophthalmoscope to the “0” position as a baseline. Note that turning towards positive numbers, often indicated in green, focuses on nearer objects, while turning towards negative numbers, sometimes in red, focuses on more distant objects.
- For the PanOptic ophthalmoscope, focus by adjusting the wheel to a point approximately 10-15 feet away.
Preparing Yourself and Your Patient

Inform your patient about the procedure. Have the patient seated and instruct them to remove glasses or contacts if worn. Explain the purpose of the ophthalmoscope and caution about the brightness of the light. If dilating the pupil with mydriatic drops, explain the process and advise on post-procedure precautions, including arranging for transportation home.
- You needn’t delve deeply into the specifics of the eye exam. Simply state, “I’ll be using this tool to examine the back of your eye. It may be bright, but it shouldn’t be uncomfortable.”

Cleanse your hands. While gloves are not mandatory, it’s customary to wash your hands thoroughly with soap and water before and after any physical examination.

Administer mydriatic drops, if needed. Widening the pupils facilitates better and more thorough examination of the eye structures, commonly practiced in optometry clinics. Have the patient tilt their head back. Gently pull down their lower lid and apply the appropriate number of drops into the eye. Instruct your patient to close their eye for approximately 2 minutes and gently press on the inner corner of their eye. Repeat this process for both eyes.
- The most frequently used is Tropicamide 0.5%, administering 1-2 drops around 15-20 minutes prior to the examination. Other agents include Cyclopentolate 1%, Atropine 1% solution, Homatropine 2%, and Phenylephrine 2.5% or 10% solution. All these drops are not recommended for patients with a monitored head injury.
- Review your patient's medication list to check for any interactions with the eye drops.
- Darker eyes may require more drops as they may be less sensitive compared to lighter-colored eyes.

Dim the room lights. Lower the light levels significantly. Excess lighting can impair the sharpness of the ophthalmoscope magnification.
- Remember, if it's not possible to darken the room, adjust the light setting on your ophthalmoscope accordingly.

Position yourself correctly in relation to your patient. Ensure you are at eye level with your patient by standing upright, leaning forward, or sitting in a chair to align with their eye level. Stand beside your patient and approach them from about a 45° angle.

Position your equipment and approach to the patient appropriately. Let's assume you're starting with the examination of the patient's right eye. Rest the ophthalmoscope against your right cheek with your right hand – when you move, your head, hand, and scope should move together. Place the heel of your left hand firmly on the patient's forehead, spreading out your fingers for stability. Gently place your left thumb over their right eye and lift the upper eyelid.
- Use your right hand and right eye to examine the patient's right eye, and vice versa.
- When using a PanOptic, stabilize the patient's head as usual and approach from 6 inches away at a 15-20° angle.
- Don't worry about getting too close to the patient during the exam. Maximum proximity is necessary for a thorough examination.

Direct your patient's gaze. Advise your patient to look straight ahead and beyond you. Directing your patient's focus to a specific point helps them relax and prevents rapid eye movements that can disrupt the examination.

Search for the crimson glow. Hold the ophthalmoscope, still positioned near your eye, at approximately arm’s length from the patient. Direct the light into the patient’s right eye at roughly a 15° angle from the eye's center, observing the pupil's response. Then, ascertain the presence of a crimson glow.
- The crimson glow refers to the reddish glimmer of light within the eye’s pupil resulting from light reflecting off the retina, akin to the glow observed in a cat's eye in dim surroundings. Absence of this glow may indicate ocular issues.
- While scanning for the crimson glow through the ophthalmoscope, minor adjustments to focus may be necessary based on your visual acuity.
Conducting the Examination

Utilize the crimson glow as a starting point for retinal examination. In a coordinated movement of head, hand, and scope, gradually track the crimson glow closer to the patient’s right eye. Halt the forward movement when your forehead touches your left thumb. Following the crimson glow should guide you toward visualizing the retina.
- Adjusting the focus of your scope may be required to bring eye features into clear view. Use your forefinger to manipulate the lens dial, if needed.
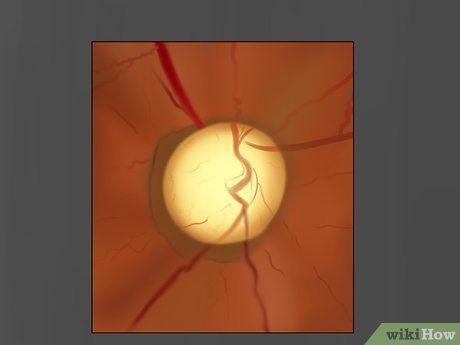
Inspect the optic nerve head. Employ a pivoting motion to maneuver the ophthalmoscope left, right, up, and down. Assess the optic disc for color, shape, contour, margin definition, cup-to-disc ratio, and status of the blood vessels.
- If locating the optic disc proves challenging, trace a blood vessel and pursue it. Blood vessels will lead you to the optic disc.
- Look for signs of cupping or swelling (edema) in the optic disc.
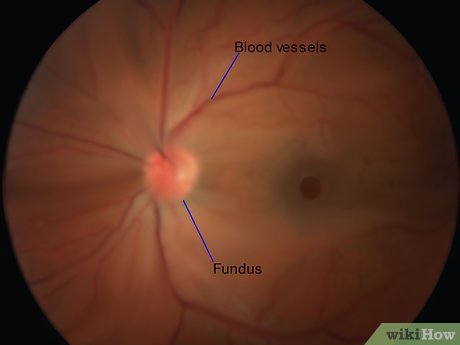
Examine the retinal blood vessels and fundus for abnormalities. Rotate to scrutinize the eye's four quadrants: upper temporal (up and outward), upper nasal (up and inward), lower temporal (down and outward), and lower nasal (down and inward). Proceed methodically, meticulously inspecting for indications of pathology. While this list is not exhaustive, remain vigilant for the following:
- AV nicking
- Hemorrhages or exudates
- Cotton wool spots
- Roth spot
- Retinal or venous occlusion
- Emboli
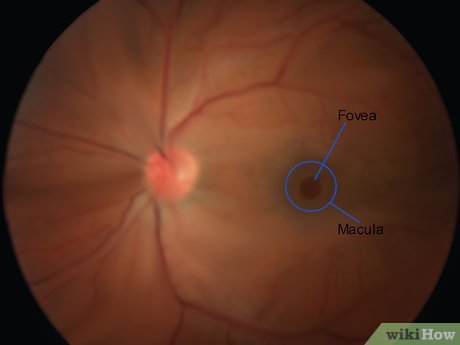
Save the assessment of the macula and fovea for last. Direct your patient to gaze directly into the light. This may cause discomfort, which is why it’s reserved for the conclusion of the examination. The macula governs central, sharp vision, making visual acuity tests pivotal in determining macular health. The macula presents as a darker disc situated roughly at the center of the retina, with the fovea appearing as a bright pinpoint within the macula.

Evaluate the other eye. Replicate the process for the opposite eye, and be sure to switch hands and eyes for the examination. While certain conditions manifest changes in both eyes, others may only manifest in one; hence, it’s crucial to meticulously observe both.

Inform your patient. Provide your patient with explanations regarding any observed abnormalities, their potential implications, and any necessary follow-up actions. If mydriatic drops were administered, advise patients about potential light sensitivity and blurred vision for several hours. Emphasize the importance of arranging transportation home and offer disposable sunglasses if needed.
Record your observations. Thoroughly document all examination findings, including detailed notes on any detected abnormalities. Incorporating visual aids, such as images, can be beneficial for recall and for tracking changes across subsequent examinations.
Insights
-
Mastering the use of an ophthalmoscope and achieving clear visualization of eye structures may initially appear daunting. This clinical proficiency demands adequate medical training and hands-on experience in identifying associated conditions.
-
Keep your non-examining eye open while using the ophthalmoscope to prevent strain.
-
Exposure to numerous images contrasting healthy and diseased eye structures is paramount for developing the ability to discern abnormalities. Familiarity with these variations enhances the capacity to identify deviations from the norm.
