Discover safe, natural, and scientifically proven methods to alleviate lichen planus symptoms.
Lichen planus is an autoimmune condition characterized by red, flat, and itchy bumps on the skin, nails, or mucous membranes in the mouth. It may also lead to hair loss. While it is not contagious and its exact cause is unknown, complete cure remains elusive. However, treatments can help alleviate discomfort. Once symptoms subside, recurrence is unlikely. Treatment typically involves symptom management, lesion healing, relief provision, and immune system enhancement. It's worth noting that while treatment may rapidly resolve symptoms for some, others may experience prolonged symptoms lasting for months or even years.
Managing Symptoms with Home Remedies

Apply anti-itch products to irritated skin. Itching is a primary discomfort associated with lichen planus. Temporary relief can be achieved by using over-the-counter anti-itch lotions and creams, typically containing antihistamines like diphenhydramine hydrochloride.
- Consult your doctor to determine the most suitable products for your specific condition.

Apply cold compresses to alleviate the bumps. For immediate relief from itching, place a washcloth soaked in cool water over the affected areas. Leaving it on for a few minutes can provide relief, especially if other treatments are slow to work or for mild cases of lichen planus.
- Avoid scrubbing the affected area to prevent further irritation.
- Ice is unnecessary as cool water is equally effective in relieving itching.

Indulge in a soothing bath. For severe symptoms or widespread bumps, consider taking a cool bath infused with soothing agents such as oatmeal. This can offer temporary relief from itching all over the body.
- Oatmeal is renowned for its anti-inflammatory properties, often used to calm inflamed skin.
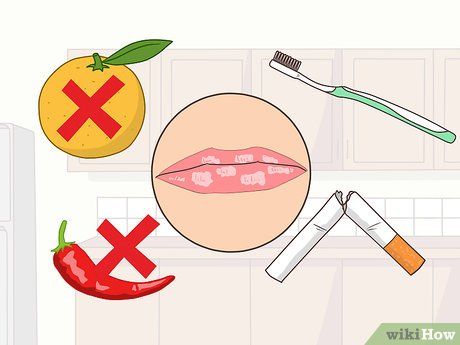
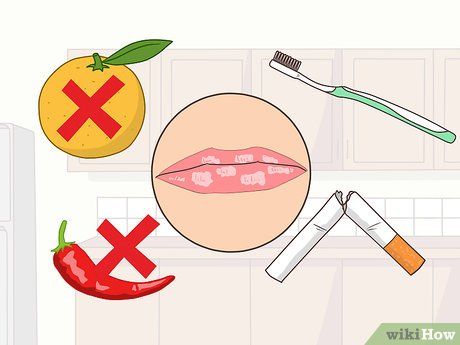
Minimize activities that aggravate oral irritation. Mouth inflammation associated with lichen planus is challenging to soothe compared to skin irritation. To reduce discomfort, refrain from smoking, maintain oral hygiene, and avoid consuming foods or beverages that can irritate the mouth, such as highly acidic or spicy items.

Allow symptoms to resolve naturally. Lichen planus often resolves spontaneously over time. Most individuals experience outbreaks for a year or two before symptoms disappear permanently. As the exact cause of the condition remains uncertain, waiting for symptoms to subside naturally is common.
- In minor cases, a small cluster of bumps may swiftly alleviate and vanish.
- While not all cases resolve without recurrence, only one in five individuals experience a subsequent outbreak.
Medical Treatment for Lichen Planus

Seek guidance from a dermatologist. Seeking care from a dermatologist, who specializes in skin conditions, is crucial if you have lichen planus. They can diagnose your condition by examining the bumps and redness on your skin or inside your mouth and provide appropriate treatment to alleviate the condition.
- In many instances, you may initially consult your primary care physician and then be referred to a dermatologist.
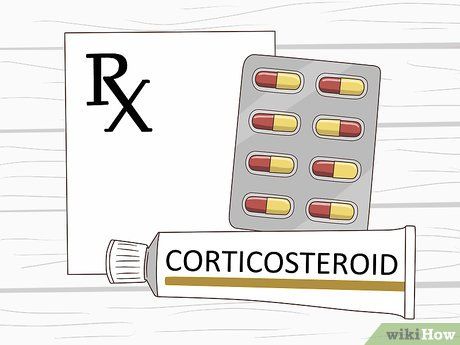
Utilize corticosteroids. Your physician will likely prescribe either topical or oral corticosteroids to treat your skin condition. These medications aid in combating the infection.
- Prolonged use of corticosteroids can lead to side effects such as changes in skin thickness and color, so they should be used for the shortest duration possible.
- Oral corticosteroids are typically recommended for lichen planus with mouth sores, as they can enter the bloodstream and treat the sores effectively. Steroids should be used for 2-4 weeks only.

Take antihistamines. If you experience severe itching, your doctor may prescribe antihistamines to alleviate the discomfort. These are usually taken orally in pill form.
- Antihistamines block the body's chemicals responsible for inflammation and irritation.
- Commonly prescribed antihistamines for lichen planus include diphenhydramine, hydroxyzine, fexofenadine, loratadine, and cetirizine.
- Be mindful that antihistamines may induce drowsiness, so read the packaging instructions and adhere to the guidelines and warnings provided.

Consider light therapy. Your dermatologist may recommend light therapy to treat your condition. Ultraviolet light treatments, such as PUVA therapy, can alleviate the rash associated with lichen planus.
- Light therapy involves applying a light-activated medication to your skin, followed by exposure to ultraviolet light to activate it.
- You may require at least 15 treatments spaced a few days apart to improve your condition.
- Consult your doctor to determine if this treatment is suitable for your specific case of lichen planus. In some situations, such as if you have sensitive skin, it may not be advisable.

Address persistent spots with dermatological intervention. As lichen planus resolves, it may leave behind stubborn dark spots. Consult a dermatologist to explore treatment options to eliminate these pigmented patches.
- Bleaching creams and laser resurfacing treatments are potential options your dermatologist may recommend to fade these spots.
Preventing Lichen Planus Outbreaks
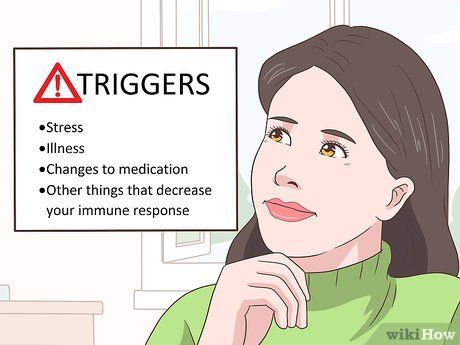
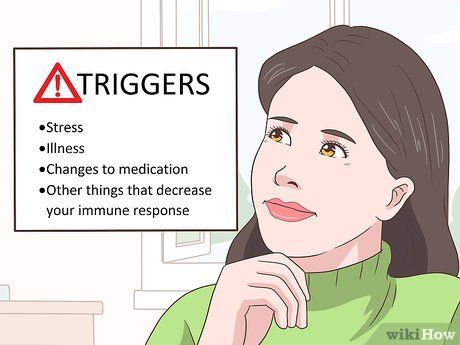
Identify and avoid potential triggers. While the exact cause of lichen planus remains unknown, understanding potential triggers, especially in recurring cases, is essential. Triggers may include stress, illness, medication changes, or other factors that weaken your immune system and increase susceptibility to outbreaks.
- Once you recognize factors that heighten your risk of an outbreak, try to avoid them whenever possible.
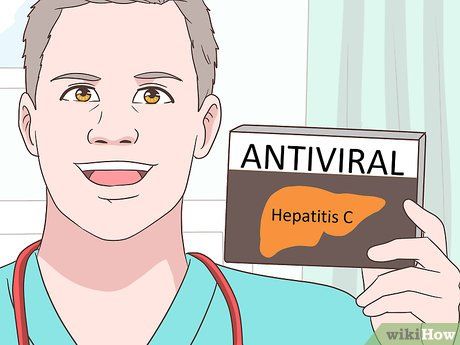
Manage hepatitis C, if applicable. Since hepatitis C is believed to contribute to certain lichen planus cases, controlling the condition is crucial. Managing hepatitis C effectively can enhance immune function and aid in eliminating lichen planus infections.
- Antiviral medications are the primary treatment for hepatitis C and should be prescribed and monitored by a healthcare professional.

Consider replacing metal fillings. If you frequently experience lichen planus infections in your mouth, it may be linked to metal fillings. Consult your healthcare provider regarding the potential replacement of metal fillings with composite alternatives.
Helpful Advice