Cellulitis is a potentially severe infection affecting the skin and soft tissues, impacting millions annually. While some cases may be minor and not warrant medical attention, a significant portion requires professional treatment. One of the most concerning aspects of cellulitis is its rapid progression from a local to a systemic infection affecting the entire body. If you suspect cellulitis, closely monitor its progression and promptly seek medical assistance if it extends beyond a localized infection.
Steps
Identifying Local Symptoms

Observe for inflammation, redness, and warmth. These are hallmark signs of cellulitis. Initially, inflammation, redness, and warmth in the affected area are likely the first indicators of infection. Vigilant monitoring is crucial. Consider:
- Inflammation and redness may be preceded by localized pain.
- Once inflammation and redness appear, closely monitor for rapid spread, as cellulitis can advance swiftly.
- If the affected area changes from red to purple or violet and expands, seek medical attention promptly.

Notice a central area swollen and possibly filled with pus. An indicative sign of cellulitis is observing a central area – the initial site of infection – swollen and abscessed, often containing pus. Treatment may involve draining the abscess in certain cases.

Report skin sensitivity and pain upon touch. Many cellulitis patients experience sensitivity when the infected area is touched. While this sensitivity or pain may start mildly, it can rapidly escalate. If pain intensifies quickly, seek medical attention.

Sense heat or warmth emanating from the infected area. A common symptom of cellulitis is warmth or heat felt upon touching the infected area. Initially subtle, this warmth can quickly escalate, causing discomfort. Additionally, radiating heat indicates spreading infection, possibly becoming systemic.
Monitoring for Systemic Symptoms
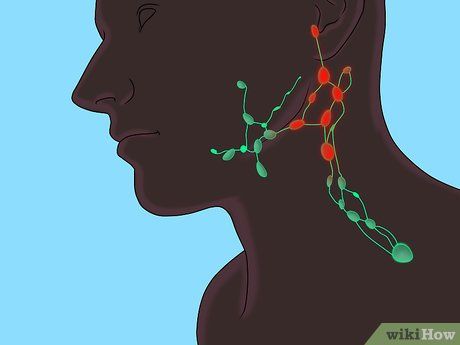
Monitor for swollen glands. Severe cellulitis cases extend beyond the initial infection site to impact the entire body systemically. Swollen lymph glands are a common systemic cellulitis sign. Note:
- Nearest lymph glands to the infection usually swell first.
- Tender and painful lymph glands are possible.
- Swollen lymph glands suggest extensive infection spread and prompt medical attention is necessary.
- Lymph nodes are found in the neck, armpits, and groin, among other areas.

Take note of fever and/or chills. While systemic symptoms vary among individuals, severe cellulitis cases may cause fever or chills. These symptoms may appear sporadically, but the severity of infection correlates with persistent fever and chills.
- Fever indicates a significant systemic infection.
- Seek immediate medical attention if cellulitis is accompanied by fever and/or chills.
- Your doctor may recommend Tylenol or other fever-reducing medications.

Experience unexplained fatigue. Individuals with severe cellulitis may feel fatigued without obvious cause, drained of energy. Fatigue is a systemic symptom indicating expanding cellulitis. Consult your doctor promptly if cellulitis is accompanied by prolonged fatigue.

Take note of unexplained sweating. Another sign of severe systemic cellulitis is unexplained sweating. Sweating may occur with or without fatigue, fever, or chills. However, sweating with cellulitis indicates infection expansion beyond the initial site.

Be aware of disproportionate pain. Serious cellulitis cases often involve intense pain disproportionate to the infection's size. If you experience severe pain with an infection, contact a doctor immediately.

Watch for lymphangitic spread. Lymphangitic spread presents as red lines extending outward from the infected area. Observing this spread suggests potentially severe cellulitis. Spread indicates infection radiating outward, potentially leading to systemic infection if untreated.
Understanding Cellulitis

Immediately address wounds to prevent infection. Prompt wound treatment is crucial as cellulitis can enter the body through open wounds. Any open wound, no matter how small, can create an opportunity for cellulitis development. Inflammation typically starts at the site of previous skin damage. Therefore, all newly opened wounds should be treated promptly. Cellulitis can be introduced by:
- Cuts
- Blisters
- Burns
- Cracks in the skin
- Surgical wounds
- Intravenous catheter insertion sites

Understand cellulitis as a bacterial infection. While cellulitis is most commonly caused by Streptococcus and Staphylococcus aureus bacteria, other types can also cause it. Blood tests and cultures are necessary to identify the bacteria responsible for cellulitis.
- If you have a known or suspected underlying condition, such as diabetes, your doctor may conduct additional tests.
- Beware of methicillin-resistant Staphylococcus aureus (MRSA), which is resistant to antibiotics. Oral antibiotics are ineffective, and intravenous vancomycin is required for treatment. Prompt treatment is essential as MRSA can become life-threatening.

Use antibiotics for cellulitis treatment. Mild cellulitis treatment involves elevating the affected area and addressing underlying conditions. Patients with edema may benefit from compression stockings or diuretics. However, antibiotics are typically the most effective treatment. Antibiotics are administered orally or intravenously depending on the severity of the affected skin area.
- For mild infections, your doctor may prescribe the oral antibiotic cephalexin. Severe cases may require vancomycin or meropenem.
- A major complication of cellulitis is infection of deeper structures, such as bones, leading to osteomyelitis, which requires aggressive treatment.
- In cases of recurrent disease, antibiotic treatment may last several months.
