Studies suggest that restoring fertility through tubal ligation reversal is feasible, although outcomes vary among individuals. This surgical procedure aims to reconnect previously blocked fallopian tubes, facilitating the passage of eggs into the uterus for potential fertilization by sperm. Success rates for conception post-reversal range from 30% to 80% within 2 years post-procedure. Factors influencing pregnancy likelihood include age, initial ligation method, fallopian tube length, and scar tissue presence. Consult your doctor for personalized expectations.
Procedures
Consulting Your Gynecologist
- Your fallopian tubes, resembling elongated ears of the uterus, facilitate egg capture from the ovary and sperm transport. Following fertilization, the embryo travels to the uterus for implantation and gestation.
- Various methods are employed for tubal ligation, none of which involve literal knotting. Common approaches include tubal rings or clips for occlusion, or tubal cauterization to induce scarring and blockage.

- The surgical area encompasses your pelvic region, presenting risks of bleeding, infection, and adjacent organ damage. Anesthesia is administered to manage pain and induce unconsciousness, albeit carrying potential adverse reactions.
- The ultimate goal of tubal reversal is achieving pregnancy. However, there's a 10% chance of ectopic pregnancy, where the fertilized egg implants outside the uterus, typically within the narrower fallopian tubes, leading to premature termination or potentially severe bleeding.

- Success hinges on scar tissue extent surrounding the tubes, necessitating disclosure of prior surgeries for conditions like endometriosis. Pelvic inflammatory disease history, denoting upper genital tract infections, also influences candidacy.
- Previous pregnancies signal fertility potential, aiding assessment. Surgical methods, such as tubal rings or partial removal, are favorable for reversals, unlike procedures like Essure or Adiana, which induce extensive scarring. Postpartum tubal ligation, especially in women under 40, is considered ideal for reversal.
- Women aged 40 and above often exhibit diminished egg quality and quantity. Follicle counting and hormone assessments gauge ovarian function. Abnormal hormone levels may impede fertility.
- Excess weight may complicate surgery and prolong anesthesia duration. BMI calculation informs about body fatness, although fertility remains unaffected.
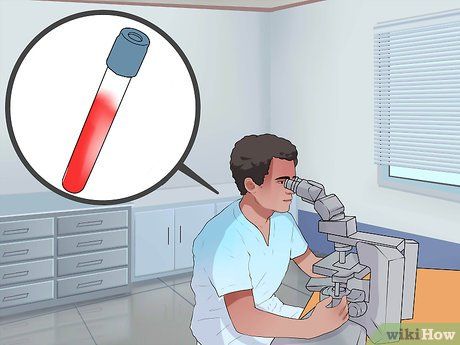
- Hysterosalpingogram assesses fallopian tube length using dye injection and fluoroscopy or ultrasound. It also evaluates ovarian health. General health insights, including cardiovascular and respiratory status, bleeding tendencies, and anesthesia reactions, optimize surgical care.

- Your partner may require referral to a urologist for further evaluation and treatment.

- IVF offers both advantages and drawbacks, making the choice between IVF and tubal reversal challenging. Factors like age, cost, time required to conceive, and the likelihood of success will be discussed with you and your partner by your doctor.
Preparing for Tubal Reversal

- Inquire about your doctor's success rate in achieving pregnancy post-reversal, ideally ranging from 40% to 85%.
- Ensure the hospital or outpatient center where the procedure will be performed is accredited, ensuring top-notch care. Accreditation is typically highlighted on the hospital's website or by the surgical center.


- Certain medications, such as aspirin, known for causing bleeding, must be discontinued several days before the tubal reversal.

- The type of soap used is not critical; the key is to cleanse the skin thoroughly to reduce bacterial presence and minimize infection risk post-surgery. Pay special attention to cleaning your belly button.
- Avoid shaving to prevent skin nicks that could lead to post-procedure infections. Leave hair removal to the trained professionals assisting in the operating room.

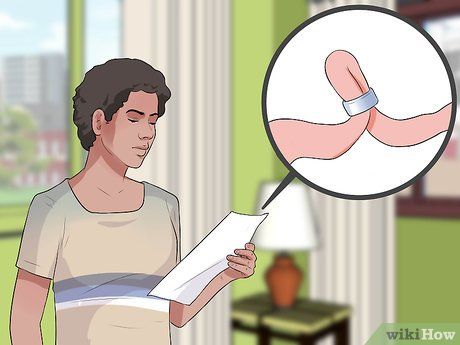
- Electrocautery, used by your doctor to control bleeding, can cause burns where jewelry contacts the skin due to its mild electrical current.
- Nail polish disrupts the pulse oximeter's ability to monitor blood oxygen levels by interfering with the light waves transmitted through the nails for measurement.
Post-Tubal Reversal Recovery

- For a laparoscopic procedure, you may return home the same or next day due to smaller incisions and less pain. Conversely, an open procedure typically requires several days of hospitalization. Pain medication will be provided upon discharge.
- Avoid lifting anything heavier than 10 to 15 pounds for 4 to 6 weeks to allow abdominal wall tissues to heal. Recovery may be faster with a laparoscopic procedure.

- Heavy vaginal bleeding, accompanied by severe abdominal pain, may indicate uncontrolled bleeding from the tubal reversal site. Excessive thirst and sweating may also signal significant blood loss.
- Nausea and vomiting could result from anesthesia or pain medication, typically resolving within 24 hours. Medications can alleviate these symptoms.
- An ileus, common after abdominal surgery, presents with symptoms like nausea, vomiting, bloating, and reduced gas passage. Symptoms should improve over time; contact your doctor if they worsen.
- Pain medications can cause severe constipation; increase fiber intake and consider a stool softener. Contact your doctor if you experience a complete cessation of gas and stool passage.

- Increased abdominal pain and fever may indicate a severe abdominal infection. Contact your doctor promptly for evaluation and appropriate treatment.
- Follow specific instructions from your doctor. Generally, wait 2 to 3 days before removing the wound dressing to allow the skin to seal and protect deeper tissues from infection. If you have a waterproof dressing, you can shower immediately; otherwise, wash around the dressing until the designated time has passed. Afterward, showering with gentle soapy water helps keep the wound clean. Avoid baths for about a month.

- The initial visit assesses your healing progress, including wound examination and pain evaluation.
- Most couples conceive within six months post-reversal. If not, your doctor may conduct a hysterosalpingogram to check tube patency. If the tubes are open, other fertility methods are explored, such as ovulation tracking, medication to enhance ovulation, or intrauterine insemination. IVF may be considered if conception challenges persist.
Tips
-
If you're considering having only one more child, IVF may be a more cost-effective option than tubal ligation reversal.
