Spinal meningitis, also known as meningitis, involves inflammation of the membranes enveloping the brain and spinal cord. While viral infections commonly cause meningitis, bacterial or fungal infections can also be responsible. The severity of meningitis varies depending on the infecting agent, ranging from easily treatable to potentially life-threatening.
Key Steps
Recognizing Symptoms in Adults and Children

Be vigilant for intense headaches. Headaches stemming from meningeal inflammation differ from other types. They are notably more severe than headaches induced by dehydration or migraines. Individuals with meningitis commonly experience persistent, severe headaches.
- Over-the-counter pain relievers often fail to alleviate meningitis-related headaches.
- If experiencing severe headaches without accompanying typical meningitis symptoms, alternative causes should be considered. Consult a physician if headaches persist for more than a day or two.

Watch for vomiting and nausea in conjunction with the headache. While migraines commonly induce vomiting and nausea, it's crucial to remain attentive to additional symptoms when experiencing such discomfort. Pay close attention to other accompanying symptoms if experiencing nausea severe enough to cause vomiting.

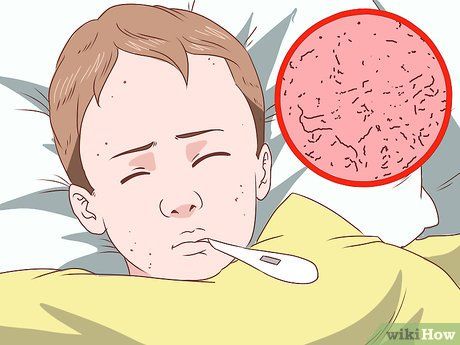
Check for fever. A high fever, combined with these symptoms, could indicate meningitis rather than influenza or strep throat. Monitor the sick individual's temperature to ascertain whether a high fever is present.
- Meningitis-related fever typically hovers around 101 degrees Fahrenheit, with any temperature exceeding 103 degrees Fahrenheit warranting concern.

Evaluate neck stiffness and soreness. This symptom is prevalent among meningitis sufferers due to pressure from inflamed meninges. Unexplained neck soreness and stiffness, unrelated to common causes like muscle strain or whiplash, may suggest meningitis.
- If neck stiffness arises, instruct the individual to lie flat on their back and attempt to flex their hips. Pain in the neck upon hip flexion indicates potential meningitis.

Be alert to difficulties in concentration. Meningitis-induced inflammation of brain membranes often leads to cognitive impairment. Inability to complete tasks, concentrate on conversations, or read through an article, coupled with severe headaches, could signify meningitis.
- The individual may exhibit unusual drowsiness and lethargy, deviating from their typical behavior.
- In rare instances, cognitive impairment may progress to varying levels of unconsciousness.

Observe for photophobia. Meningitis in adults is associated with eye pain and sensitivity to light, resulting in photophobia. Difficulty tolerating sunlight or bright indoor lighting may indicate meningitis.
- Initially, this sensitivity may manifest as a general discomfort or avoidance of bright lights. Monitor for this behavior alongside other symptoms.

Watch for seizures. Seizures involve involuntary muscle movements, often violent, typically resulting in loss of bladder control and disorientation. Following a seizure, individuals may experience confusion regarding their surroundings and personal information.
- For individuals with epilepsy or a seizure history, seizures may not indicate meningitis.
- If witnessing a seizure, immediately call emergency services. Safely position the individual on their side and remove nearby objects to prevent injury. Seizures typically cease within one to two minutes.

Look for the distinctive rash. Specific types of meningitis, such as meningococcal meningitis, manifest with a distinct rash. This rash appears reddish or purple, often blotchy, and may indicate blood poisoning. To assess for meningitis, perform the following glass test:
- Press a clear glass against the rash to observe the skin beneath.
- If the skin remains unaffected under the glass, blood poisoning may be present. Seek immediate medical attention.
- Not all meningitis variants exhibit a rash. Lack of rash does not rule out meningitis.
Observing Meningitis Signs in Infants
Recognize diagnostic difficulties. Identifying meningitis in children, especially infants, poses challenges even for experienced pediatricians. Similar presentations of benign viral syndromes, characterized by fever and infant distress, complicate meningitis diagnosis in young children. Consequently, clinicians often maintain a high index of suspicion for meningitis, particularly in infants under three months with limited vaccination history.
- Effective vaccination efforts have reduced bacterial meningitis cases. Although viral meningitis persists, its presentation tends to be mild and self-resolving, necessitating minimal intervention.

Assess for elevated body temperature. Infants, like older individuals, commonly develop fevers in meningitis cases. Monitor your baby's temperature and seek medical attention if fever is present. Regardless of the cause, prompt medical evaluation is essential for feverish infants.

Monitor for persistent crying. Although various illnesses can trigger crying in babies, if your infant appears unusually distressed and remains inconsolable despite typical soothing methods, seek medical attention. Persistent crying, coupled with other symptoms, could indicate meningitis.
- Meningitis-related crying often defies comfort measures. Look for deviations from the baby's typical crying patterns.
- Some parents note that infants become more agitated when picked up if meningitis is the cause.
- Meningitis may elicit a higher-pitched cry than usual.

Observe for drowsiness and reduced activity. A lethargic, drowsy, irritable infant displaying decreased activity levels may signal meningitis, particularly if this behavior contrasts with their typical active state.

Take note of weak sucking during feeding. Infants affected by meningitis may exhibit diminished sucking ability during feedings. Promptly contact a healthcare professional if your baby struggles with sucking motions while feeding.

Watch for alterations in the baby's neck and body movements. Difficulty in head movement and apparent stiffness in the body may indicate meningitis. Pay attention to observable changes suggestive of decreased mobility and discomfort.
- The infant may exhibit neck and back pain, initially presenting as stiffness. If movement causes distress, the condition may be severe. Observe for involuntary leg movements towards the chest when bending the neck forward or signs of discomfort when flexing the legs.
- Inability to straighten the lower legs with hips at a 90-degree angle is common, particularly noticeable during diaper changes.
Exploring Different Meningitis Types
Explore viral meningitis. Viral meningitis typically resolves on its own and is often caused by viruses like herpes simplex virus (HSV) and HIV, necessitating specific antiviral therapy. It spreads through person-to-person contact, primarily via enteroviruses, commonly during late summer to early fall.
- Although viral meningitis can spread through person-to-person contact, outbreaks are infrequent.

Discover Streptococcus pneumoniae. Bacterial meningitis, the most dangerous form, is caused by three types of bacteria. Streptococcus pneumoniae is the predominant cause in the US, affecting infants, children, and adults. However, vaccination offers a cure. It typically stems from sinus or ear infections, especially when meningitis symptoms develop after such infections.
- Individuals lacking spleens or aging individuals are at heightened risk and require vaccination.
Grasp Neisseria meningitidis. Another bacterium responsible for bacterial meningitis is Neisseria meningitidis. Highly contagious, it affects healthy adolescents and young adults, often leading to severe complications like multi-organ failure and brain damage. Transmission occurs person-to-person, with outbreaks common in schools and dormitories.
- This bacterium can cause a distinctive 'petechial' rash resembling tiny bruises, a key diagnostic indicator.
- Vaccination is recommended for adolescents aged 11 to 12, with a booster at 16, or a single vaccination for unvaccinated 16-year-olds.
Acquaint yourself with Haemophilus influenza (Hib). Haemophilus influenza was once a leading cause of bacterial meningitis in children until the introduction of Hib vaccination, resulting in a significant decline in cases. However, populations with incomplete vaccination histories remain susceptible due to factors like immigration or vaccine hesitancy.
- Accurate vaccination records, ideally from medical records or vaccination cards, are crucial for meningitis diagnosis, including Hib.

Understand fungal meningitis. Fungal meningitis, rare and primarily affecting individuals with AIDS or weakened immune systems, is considered an AIDS-defining condition. Cryptococcus is the usual culprit, and prevention involves maintaining low viral loads and high T-cell counts through antiretroviral therapy in HIV-infected individuals.
- For HIV-infected individuals, compliance with antiretroviral therapy is essential for preventing fungal meningitis and other opportunistic infections.
Consider meningitis vaccines when necessary. Certain high-risk groups are advised to receive routine vaccinations against meningitis:
- All individuals aged 11-18
- U.S. military recruits
- Individuals with a compromised or absent spleen
- First-year college students residing in dormitories
- Microbiologists exposed to meningococcal bacteria
- Individuals with terminal complement component deficiency (a disorder of the immune system)
- Travelers to countries experiencing meningococcal disease outbreaks
- Those potentially exposed to meningitis during an outbreak
