Psychiatric patients, despite their challenges, deserve compassion and assistance throughout their treatment. Although it can be frustrating to handle them and there will be tough days, there are constructive approaches to engaging with them and fulfilling their needs. It's also possible to defuse aggressive behavior if needed. If a loved one is the patient, there are various support options available.
Steps
Engaging with Patients
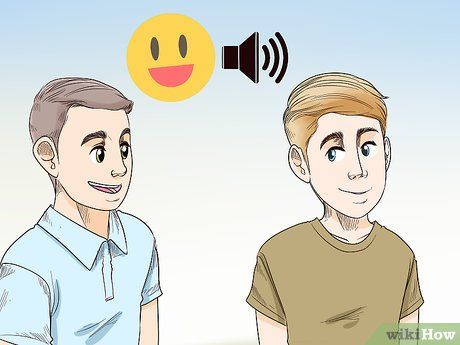
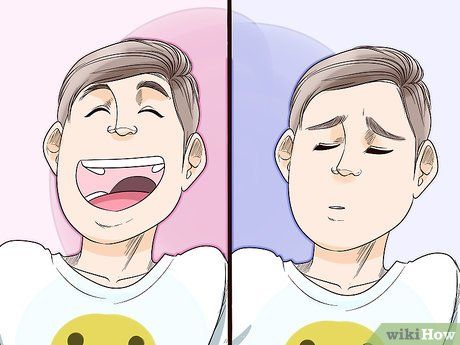
Adopt a warm, yet professional demeanor. Patients should perceive your authority without feeling patronized. A friendly tone communicates care, while maintaining professionalism indicates confidence in their treatment and control of the situation.

Focus on the patient's treatment plan, not personal opinions. Patients may exhibit behaviors you disagree with, but avoid expressing your judgments. Follow their treatment plan and assist them in their recovery journey, regardless of your opinions.
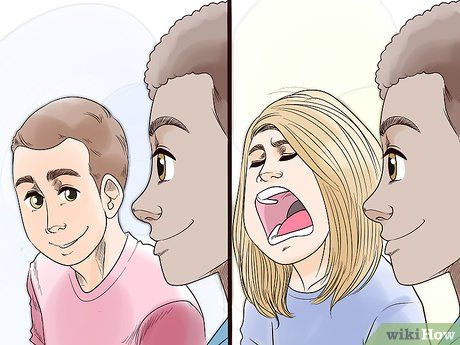
Treat all patients equally. Some patients may be more challenging, but it's crucial to treat them with the same respect and care as others. This approach not only fosters fairness but also enhances the treatment process.
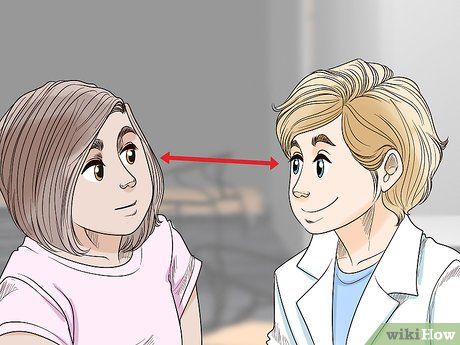
Maintain natural eye contact when speaking. Natural eye contact conveys openness and honesty, reinforcing the patient's sense of equality. Avoid staring, as it may be perceived as demeaning.

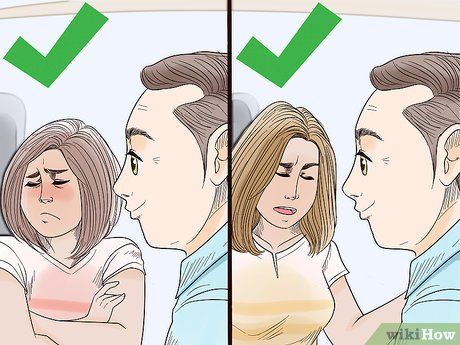
Utilize open body language to prevent negative reactions. Patients can sense hostility in body language, so adjust yours to appear non-threatening. Maintain good posture, keep arms relaxed, and wear a neutral or friendly expression.

Respect the patient's personal space unless necessary. Unless in an emergency, build trust before invading personal space. Even then, prioritize respecting boundaries. Approach gently, asking permission before entering their space.

Limit physical contact with patients, unless absolutely necessary. Some patients may find touch distressing, possibly due to their condition. Always obtain consent or consider medical necessity before touching a patient.
Addressing Patient Needs

Listen attentively to the patient's concerns. Patients feel valued and are less likely to act out if they believe they are being heard. Even if their concerns seem irrational or symptomatic, validate their feelings by actively listening and summarizing their statements.

Show empathy in your responses to the patient. Expressing empathy reassures the patient that their feelings are acknowledged and understood. This not only aids in calming them but also fosters a therapeutic connection.

Offer the patient choices. When faced with resistance, presenting options empowers the patient and guides them toward desired outcomes. Incorporate their preferences into treatment plans to increase compliance and a sense of control.

Customize treatment according to the patient's personality. Understanding each patient's personality facilitates effective treatment. Four personality types—dependent, histrionic, antisocial, and paranoid—affect treatment acceptance and approach.

Avoid deception to gain patient compliance. While lying may seem expedient, it erodes trust and exacerbates resistance. Patients must trust their providers for successful treatment outcomes, except when managing delusions.
Provide equitable care for psychiatric patients. Overcoming biases against psychiatric patients ensures they receive necessary care. Negative perceptions can lead to premature discharge and hinder recovery.

Maintain comprehensive documentation. Detailed records are vital for quality care, encompassing diagnosis, treatment, and symptom recurrence. Thorough documentation safeguards against malpractice claims and aids in tailored care.
Engage patient relatives in treatment where feasible. Involving relatives enhances patient outcomes, though HIPAA laws may limit participation. Encourage their involvement through family therapy sessions or sharing treatment plans, particularly for post-discharge support.
Addressing Aggressive Behavior
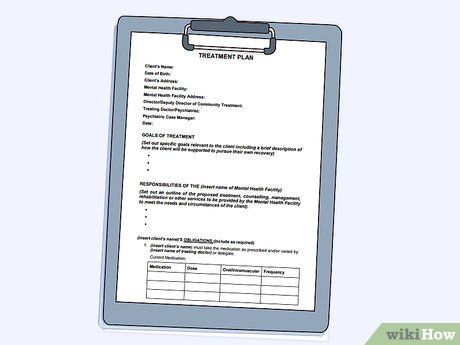
Refer to the patient's treatment plan. Reviewing their plan can offer insights into de-escalation strategies tailored to their needs. In urgent situations, prioritize safety over consulting the plan.

Relocate the patient to a calm, secluded area. Providing space allows for self-calming, particularly beneficial for overwhelmed patients.

Secure or remove potentially harmful objects. Protecting everyone involved is paramount; prioritize removing items that could cause harm.
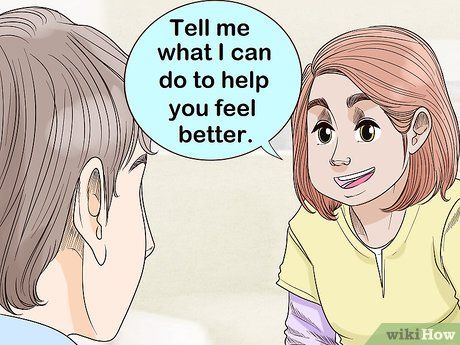
Validate their emotions to foster communication. Avoid invalidating their feelings, which can exacerbate the situation. Instead, acknowledge their emotions and offer support.

Avoid making threats. Threatening consequences for not calming down can escalate aggression. Instead, offer assistance and support without resorting to punitive measures.

Consider administering medication if necessary to alleviate agitation. In cases where verbal de-escalation is insufficient, medication may be required. Administering medication without restraint is ideal.

Resort to physical restraint only as a last resort. Restraining should be conducted by trained personnel in a hospital setting, as it can pose risks. It's primarily utilized to facilitate the administration of calming medication.
Coping with a Loved One's Mental Health Condition
Educate yourself about their condition. Research online, consult literature, and communicate with their healthcare provider to gain insight into their condition. Engage in open discussions with your family member if they're comfortable sharing.

Offer your support for their recovery journey. Assure them of your presence and willingness to help them through their healing process, even if it involves lifelong management of their symptoms and relapses. Communicate your readiness to assist with their treatment plan if they're comfortable with it.

Use 'I' statements when addressing relationship issues. When discussing concerns, express them from your perspective rather than blaming the other person. This fosters constructive communication without placing blame.
Adjust your expectations regarding their recovery. Recognize that managing their illness may be a lifelong journey, even with treatment. Avoid pressuring them to conform to societal norms or take on excessive responsibilities to prevent conflict and setbacks.

Join a support group to enhance coping mechanisms. Engaging with individuals facing similar challenges provides emotional support and practical advice. Seek recommendations from healthcare professionals or online resources for suitable support groups.
Assisting Communication with Patients
 Effective Strategies for Communicating with Psychiatric Patients
Effective Strategies for Communicating with Psychiatric Patients