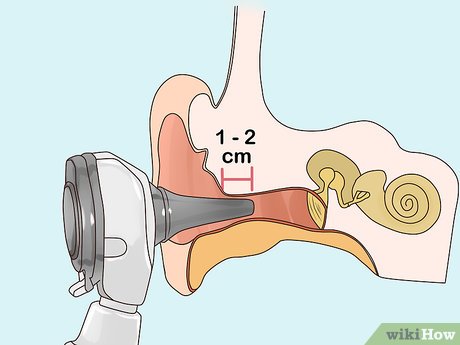
An otoscope serves as a vital tool in a doctor's arsenal, facilitating a comprehensive examination of the ear. By magnifying the inner ear, it aids in identifying common issues such as Swimmers ear and excessive earwax accumulation. Typically equipped with a magnifying lens, a cone-shaped speculum attached to a tube, and an illuminating source, this instrument may also be employed to inspect the throat or nasal passages. Utilizing an otoscope involves activating the light source and grasping the device between thumb and forefinger, akin to holding a pencil. Gently lifting the outer ear to align the ear canal, the otoscope is then inserted approximately 1-2 cm (0.4-0.8 in) into the canal for examination.
Procedures
Preparing Yourself and the Patient
- Solicit feedback from the patient regarding comfort levels, ensuring to adjust pressure accordingly. For instance, inquire, “Mr. Neumaier, is the pressure tolerable? Please notify me of any discomfort.”

- Your supporting hand acts as a safeguarding lever in case of sudden head movements by the person.

- For infants and children under 3 years old, pull the outer ear downward.
- When examining the right ear, grasp the ear at the 10 o’clock position; for the left ear, grasp at the 2 o’clock position.
Ear Examination Procedure
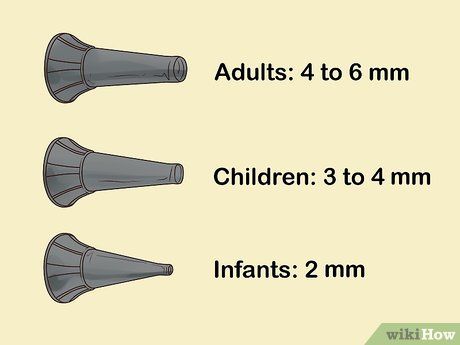
- Adults: 4 to 6 millimeters
- Children: 3 to 4 millimeters
- Infants: as small as 2 millimeters


- Avoid applying excessive pressure to the otoscope, which may cause discomfort by striking the inner canal wall.



- If disposable speculums are unavailable, cleanse each tip with hot water to remove excess wax. Subsequently, immerse the speculum in a covered container of rubbing alcohol for 10 minutes.
Spotting Potential Issues
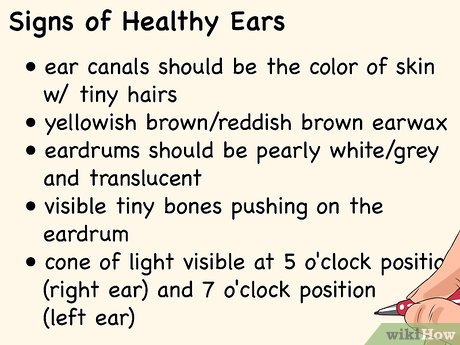
- The ear canal should exhibit skin-like coloration with fine hairs, accompanied by normal yellowish or reddish-brown earwax. Swelling should be absent.
- The eardrum should appear pearly white or gray, with translucency. Observable features include tiny bones pressing against the eardrum and a visible cone of light at the 5 o'clock position in the right ear and the 7 o'clock position in the left.
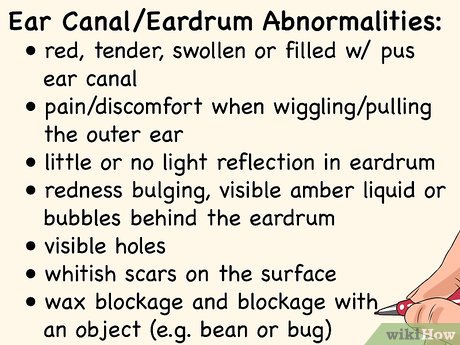
- Pain or discomfort upon manipulation of the outer ear, accompanied by redness, tenderness, swelling, or pus in the ear canal.
- The eardrum may lack light reflection, exhibit redness, bulging, visible amber fluid or bubbles behind it, holes, whitish scars, wax blockage, or foreign object impaction.

- Inflammation
- Redness
- Swelling
- Pus
- Dull or red eardrum
- Fluid or bubbles behind the eardrum
- Eardrum perforation
- Foreign objects or impacted wax
References
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK556090/
- ↑ https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=zm2528
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK556090/
- ↑ https://www.mottchildren.org/health-library/hw227459#aa37178
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317759/pdf/jathtrain00025-0054.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317759/pdf/jathtrain00025-0054.pdf
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK556090/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317759/pdf/jathtrain00025-0054.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1317759/pdf/jathtrain00025-0054.pdf
- ↑ https://nhsna.wildapricot.org/resources/Pictures/HOW%20TO%20USE%20AN%20OTOSCOPE.pdf
- ↑ https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_au.pdf
- ↑ https://my.clevelandclinic.org/health/articles/13076-ear-care-tips
- ↑ https://my.clevelandclinic.org/health/articles/13076-ear-care-tips
- ↑ https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media
Useful Tips
Important Warnings
- Exercise caution when using an otoscope. Your physician has undergone proper training in techniques to mitigate the risk of injury resulting from improper usage.
