Ensuring your pancreas's well-being holds significant importance for your overall health, especially following an episode of acute pancreatitis. Adopting lifestyle adjustments such as embracing a nutritious diet, shedding excess weight, and steering clear of alcohol and tobacco can alleviate discomfort associated with chronic pancreatitis and impede disease progression. Additionally, your healthcare provider might propose medical interventions to facilitate pancreas healing or forestall further complications.
Procedures
Implementing Lifestyle Alterations

Embrace a balanced, low-fat diet. Opting for a nutritious diet can mitigate abdominal discomfort and lighten the workload on your pancreas, enabling it to recuperate from inflammation. A pancreas-friendly diet should emphasize ample servings of vegetables, fruits, whole grains, legumes, low-fat or fat-free dairy products, and lean meats. Consuming small, frequent meals can expedite your recovery.
- Dark leafy greens, blueberries, sweet potatoes, carrots, grapes, and walnuts offer particularly favorable benefits.
- Incorporate animal-based omega-3 fatty acids, such as those found in salmon, into your dietary regimen.
- Garlic and probiotic-rich foods, like yogurt, possess anti-inflammatory properties and aid in digestion.
- Following a Mediterranean diet can accelerate your pancreas's recuperation.
- Aim for 6-8 small, protein-rich meals per day instead of three large ones.
- Following pancreatitis treatment, your healthcare provider may provide tailored dietary guidance.
- Avoid crash diets that involve extreme calorie restriction for weight loss.
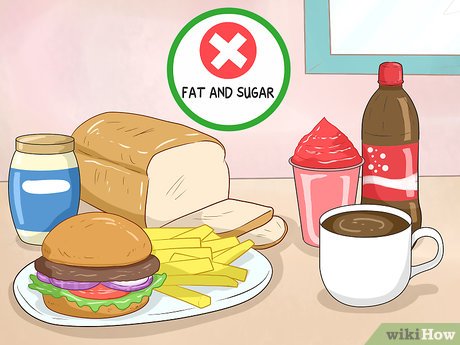
Avoid consuming foods rich in fat and sugar. Foods high in fat and simple sugars elevate blood fat levels, heightening the risk of pancreatitis. Since the pancreas metabolizes most dietary fat, steering clear of high-fat foods can alleviate its workload and expedite recovery.
- Strive to limit daily fat intake to 30 grams or less.
- Reduce consumption of red meat, organ meat, French fries, mayonnaise, butter, pastries, white bread, pasta, and sugary beverages.
- Avoid fried, processed, or greasy foods to minimize fat intake.
- If feasible, eliminate caffeine from your diet.

Focus on weight loss to alleviate pancreatic stress. Obesity diminishes insulin sensitivity, necessitating increased insulin production by the pancreas to maintain blood sugar levels.
- Even modest weight loss of 5–10 pounds (2.3–4.5 kg) can alleviate pancreatic stress.
- Weight loss may also mitigate gallstone formation, a pancreatitis risk factor.

Refrain from excessive alcohol consumption. Minimize alcohol intake to safeguard pancreatic health. If necessary, consume alcohol in moderation, with a limit of 2 drinks per day for men and 1 for women.
- Avoid alcohol entirely if diagnosed with acute or chronic pancreatitis.
- Continued alcohol consumption post-acute pancreatitis diagnosis may exacerbate the condition, leading to chronic pancreatitis.
- For individuals with chronic pancreatitis, alcohol consumption may result in severe complications, including death.

Make efforts to quit smoking to reduce pancreatitis risk. Smoking heightens pancreatitis risk, particularly when combined with alcohol consumption. Quitting smoking is crucial for diagnosed pancreatitis patients, as it can mitigate disease severity.
- Smoking with pancreatitis elevates pancreatic cancer risk, emphasizing the importance of smoking cessation.
- Supplementing with enzymes may alleviate symptoms like fatty diarrhea, bloating, and abdominal pain.
Treating Pancreatitis

Seek immediate medical attention upon noticing pancreatitis symptoms. Severe symptoms may include intense abdominal pain, nausea, vomiting, fever, rapid heartbeat, shortness of breath, and yellowing of the skin or eyes. These indicators may signal a serious infection, inflammation, or pancreatic blockage.

Undergo supervised fasting as per your doctor's guidance. If hospitalized for pancreatitis treatment, your doctor might advise fasting for a couple of days. This fasting period allows your pancreas to rest and recuperate, potentially reducing inflammation.
- Following fasting, you may transition to clear liquids and bland foods before resuming your regular diet.

Use pancreatic enzyme supplements to enhance digestion. Individuals diagnosed with chronic pancreatitis may require enzyme supplements with meals to aid nutrient absorption.
- Your doctor may prescribe pancreatic enzymes if deemed beneficial for your condition.

Discuss gallbladder surgery if pancreatitis stems from gallstones. Gallstones commonly trigger pancreatitis. If gallstones are the cause, your doctor may recommend gallbladder removal to prevent future occurrences.
- Cholecystectomy, the gallbladder removal surgery, is routine with minimal risk of complications. Typically, patients return home on the same day, requiring about a week for full recovery.

Consult your doctor regarding the necessity of pancreas surgery. In severe cases, surgery may be advised if pancreatitis persists despite antibiotic treatment or to remove damaged pancreatic tissue.
- Pancreatic surgery is a significant procedure, considered only after exhausting alternative treatments.

Clear bile or pancreatic duct blockages with ERCP. ERCP (endoscopic retrograde cholangiopancreatography) is employed by doctors to extract gallstones obstructing bile or pancreatic ducts. This procedure is utilized in treating both acute and chronic pancreatitis.
- ERCP may induce acute pancreatitis in certain individuals.
Suggestions
-
Consider meditation or yoga practice to alleviate stress and pain.
-
During acute pancreatitis, prioritize rest to mitigate symptoms.
