As you journey to higher elevations, particularly mountainous regions, you'll encounter various environmental changes that can impact your well-being. These include cold temperatures, low humidity, increased sun exposure to UV radiation, decreased air pressure, and diminished oxygen levels. Altitude sickness arises as a response to the reduced air pressure and oxygen levels typically experienced at altitudes exceeding 8,000 feet. If you anticipate traveling to such heights, adhere to some simple strategies to prevent altitude sickness.
Guidelines
Strategies for Preventing Altitude Sickness

- It's essential to avoid certain behaviors. Do not exceed 9,000 feet in altitude in a single day. Avoid sleeping at an elevation 1,000 to 2,000 feet higher than the previous night. Allocate an extra day for acclimatization for every 3,300 feet gained.

- Furthermore, during your three to five-day adjustment period to the new altitude, prioritize rest for the initial days before engaging in exploratory activities.

- Acetazolamide is an FDA-approved medication for preventing and treating acute mountain sickness. It functions as a diuretic, increasing urine production, and enhances respiratory ventilation, facilitating greater oxygen exchange in the body.
- Follow the prescribed dosage of 125 mg twice daily, commencing one day before your trip and continuing for two days at your highest altitude.

- Administer as directed, typically 4 mg every 6 to 12 hours commencing the day prior to your journey and continuing until full acclimatization at your highest altitude.
- Additionally, consuming 600 mg of ibuprofen every 8 hours may aid in preventing acute mountain sickness.
- While Ginkgo biloba has been studied for altitude sickness treatment and prevention, its efficacy remains inconsistent, and it is not recommended for use.
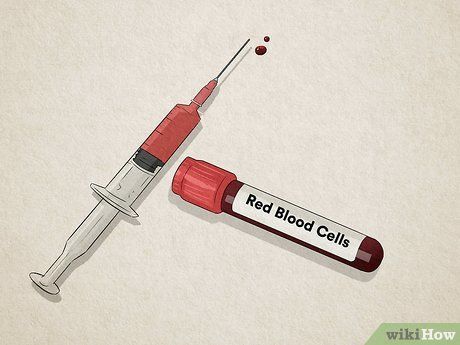
- Low RBC count can result from various factors, with iron deficiency being the most common. Deficiency in B vitamins can also contribute to low RBC levels. If deficient, your doctor may suggest iron or vitamin B supplements to correct the imbalance.
- Avoid consuming alcohol, and refrain from doing so for the initial 48 hours of your trip. Alcohol acts as a depressant, slowing breathing rate and promoting dehydration.
- Similarly, avoid caffeinated beverages such as energy drinks and sodas, as caffeine can lead to muscle dehydration.

- This may include pastas, breads, fruits, and potato-based meals.
- Avoid excessive salt intake, as it can lead to dehydration of body tissues. Look for foods and meals labeled as low-salt or no-salt-added at the grocery store.
- While physical endurance and conditioning may seem beneficial before mountain climbing, studies indicate no evidence that physical fitness guards against altitude sickness.
Identifying Symptoms

- Acute mountain sickness results from decreased air pressure and oxygen levels.
- HACE represents a severe progression of acute mountain sickness, characterized by brain swelling and dilated brain vessel leakage.
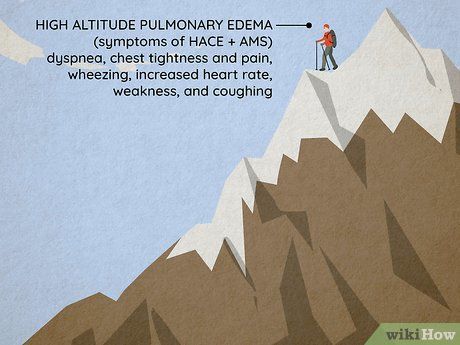
- HAPE may occur independently or accompany HACE, or develop one to four days after ascending above 8,000 feet. It involves lung swelling due to fluid leakage caused by high pressure and blood vessel constriction in the lungs.
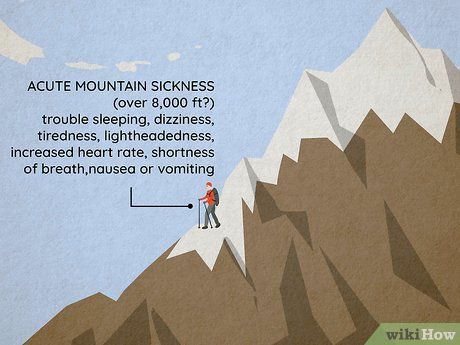
- Recognizable symptoms encompass headache within two to 12 hours of altitude change, sleep disturbances, dizziness, fatigue, increased heart rate, shortness of breath during activity, and nausea or vomiting.
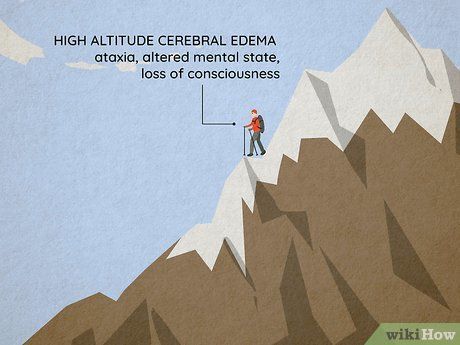
- Unlike acute mountain sickness, HACE is relatively rare, affecting only 0.1% to 4% of individuals.
- You may also observe physical changes such as cyanosis, where the mouth and fingers turn darker or bluish in color.
- Similar to HACE, HAPE is relatively rare, occurring in only 0.1% to 4% of cases.
- If experiencing signs of HACE or HAPE, descend immediately with minimal exertion to avoid worsening symptoms. Periodically reassess symptoms for improvement.
- If descent isn't feasible due to weather or other constraints, administer oxygen to increase pressure. Utilize portable hyperbaric chambers if available. If symptoms are manageable and respond to treatment, descent may not be necessary. Report incidents to rescue teams if communication is possible, providing location details and awaiting assistance.

- For HAPE, your doctor may prescribe non-FDA approved drugs for prophylaxis and treatment. Some studies suggest these drugs can reduce HAPE incidence if taken 24 hours before the trip. Options include nifedipine (Procardia), salmeterol (Serevent), and phosphodiesterase-5 inhibitors (tadalafil, sildenafil).
Dietary Recommendations
 Foods That Aid in Altitude Sickness Prevention
Foods That Aid in Altitude Sickness Prevention Foods to Steer Clear of to Prevent Altitude Sickness
Foods to Steer Clear of to Prevent Altitude SicknessUseful Advice
Key Warnings
- If you're experiencing symptoms of altitude sickness, avoid further ascent, especially for sleeping.
- Descend if your symptoms worsen or persist despite resting.
- If you have certain medical conditions, they may worsen at high altitudes. Consider a pre-trip evaluation by your healthcare provider for safety. These conditions include arrhythmias, severe COPD, congestive heart failure, coronary artery disease, hypertension, pulmonary hypertension, diabetes, and sickle cell disease. Additionally, be cautious if you're taking narcotic pain medications, as they can reduce respiration.
- Pregnant women should avoid sleeping at altitudes above 12,000 feet.
