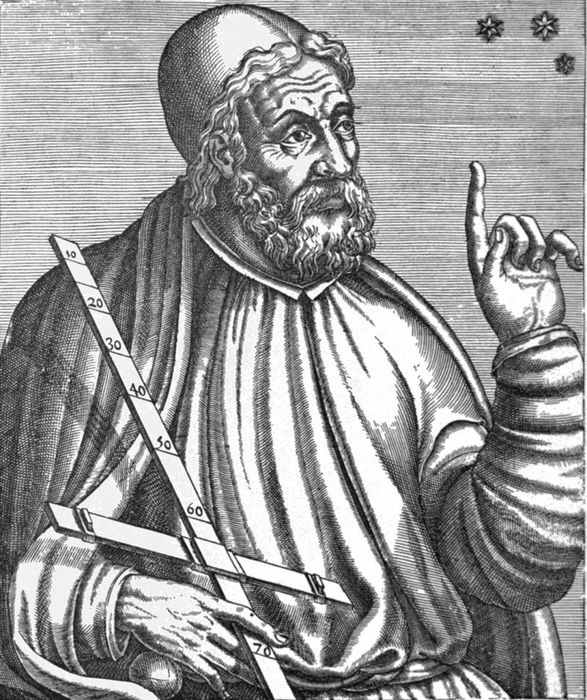
1. Ancient Physician Hippocrates - The Father of Medicine
Hippocrates - the father of modern medicine and considered the greatest physician of his era. He authored the 'Hippocratic Oath' which is still used in many countries including Vietnam. It is recited and pledged by medical students upon graduation to practice ethically.
He practiced medicine based on observations and studies of the human body. According to him, the body needs to be viewed as a whole rather than a collection of discrete parts. And each disease has a cause, rejecting the belief that diseases are due to sinful thoughts or disloyalty to God. He was the first to describe symptoms of pneumonia, epilepsy in children. He believed in the natural healing process through rest, proper nutrition, fresh air, and cleanliness. Therefore, he observed that each person would manifest different disease symptoms, different disease resistance abilities. He was also the first physician to believe that human thoughts, emotions originate from the brain, not from the heart as many contemporaries believed.
Today, most of what is known about medical practices comes from a collection of over 60 medical books known as the Hippocratic Corpus, considered the oldest medical works. The collection was compiled 100 years after his death. Historians believe that the documents helped physicians in their medical practice throughout their lives. Hippocrates' works advocate healthy eating habits and physical exercise as effective remedies for most diseases. Hippocrates identified joint positioning, the importance of maintaining records of medical history and treatment, the relationship between weather and some diseases. Physicians at that time only observed patients based on what could be seen or felt externally. They also experimented on animals to compare with humans, but never experimented on deceased humans.
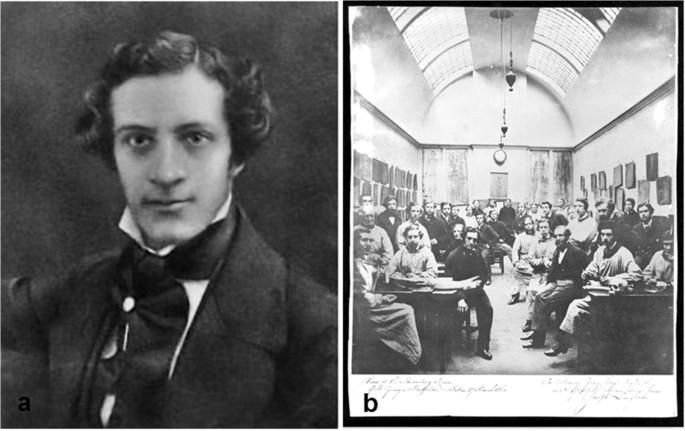
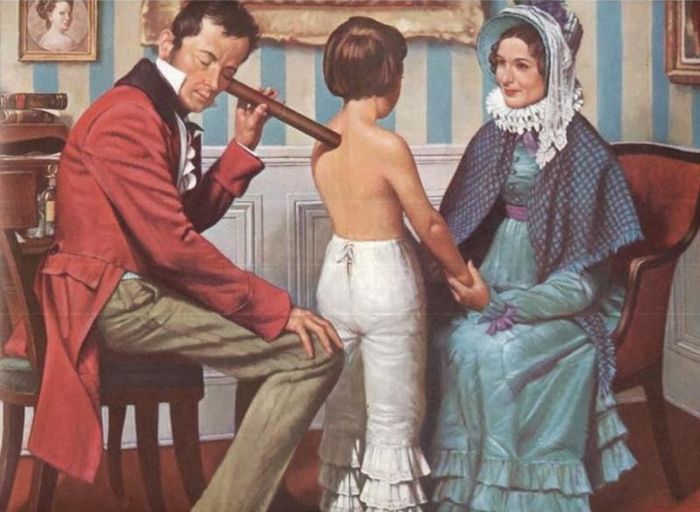
2. Physician Rene Laennec - Inventor of the Stethoscope
Rene Laennec was born in 1781, in France, ranked 52,065th worldwide and 61st on the list of Famous Physicians. He invented the stethoscope during the care of an overweight patient whose heartbeat could not be heard or felt, devising a tool to amplify the sound of the heartbeat, which became the stethoscope.
Thanks to Laennec's invention of the stethoscope, diagnosing and examining patients became more effective. Wooden stethoscopes were used until the latter half of the 19th century, after which the stethoscope underwent numerous improvements and became increasingly popular. Nowadays, rubber stethoscopes are commonly used, allowing physicians to hear sounds within the patient's body at low and high frequencies. In medicine, the stethoscope for heartbeats is a simple combination of one of the most basic laws of physics, sound transmission and amplification. However, it has a significant impact and has become an icon of modern medicine. Initially intended to create a distance between physicians and patients, the stethoscope has now become a distinctive tool for physicians and is useful in serving patients.
In the final months of his life, he requested his grandson, Mériadec, to stimulate his chest and describe what he heard with the stethoscope. He died from pulmonary tuberculosis, the disease that Laënnec himself illuminated with his stethoscope. In his will, Laënnec bequeathed all his medical research to his grandson, along with the wooden stethoscope, a more valuable relic than anything else.

3. Physician Edward Jenner - The Father of Vaccination
Today, the world recognizes vaccination as the most effective method of disease prevention. This medical achievement has helped nearly 8 billion people worldwide avoid death from epidemics that ravaged prior to the 17th century. Vaccination is applied to both adults and children, and almost everyone understands that with just one shot, our bodies become immune to many deadly diseases.
In the minds of many, Louis Pasteur is thought to be the father of vaccines because he is so famous for discovering bacteria, infections, and producing vaccines against rabies. In reality, Pasteur is not the father of vaccines; that credit belongs to an honorary physician of the Royal Society of London. It was Edward Jenner who demonstrated the effectiveness of vaccines in disease prevention for humanity before the world knew of the existence of viruses and bacteria. The world medical history acknowledges Edward Jenner's significant contribution in establishing the vaccine empire, protecting billions of people worldwide.
In 1796, Europe was in the grip of a smallpox epidemic. At this time, no one had any concept of viruses. In 1798, when Dr. Edward Jenner announced the results of his vaccination experiments, people of that era began to imagine the existence of infectious 'germs.' Smallpox had appeared for a long time in human history, becoming an epidemic from the 6th century, originating from Africa, and later spreading to Europe and Asia.
In the 17th and 18th centuries, the disease claimed the lives of millions. Smallpox was caused by a virus, but doctors living before Louis Pasteur's time had no concept of this issue; they believed it was an incurable disease. It wasn't until 80 years later that Louis Pasteur discovered bacteria. Jenner's greatest success was conquering smallpox. In 1802, he was elected Chairman of the International Commission for the Eradication of Smallpox. The physician was successively awarded by the Queen of England, Russia, the Emperor of France, and the President of the United States for his significant contributions to humanity.


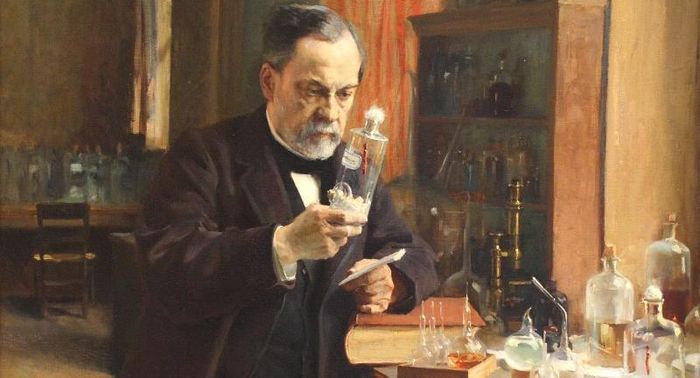
4. Physician Louis Pasteur - Discoverer of Rabies Vaccine
Louis Pasteur was born on December 27, 1822, in the city of Dole in western France. He graduated with honors from Besancon University (France). He then continued his studies in physics and chemistry at the University of Paris, and successfully defended his doctoral thesis.
He completed his greatest works, such as identifying the causes of infectious diseases in animals such as avian plague, rabies, and developing vaccines to prevent diseases such as avian plague, anthrax, and especially rabies. In just one year, with this success, over 2,500 people bitten by rabid dogs were vaccinated and saved. The first trial of rabies vaccine on humans made Louis Pasteur very anxious. He wrote a letter to his son: 'Imagine how much pain your father's heart would be torn apart if he had to witness a life lost because of your father's vaccine.'
In 1868, Pasteur received a medical degree from Bonn University (Germany) and was awarded the Bavarian Order of Merit. Unfortunately, he later became paralyzed on one side, but the scientific spirit within him remained vigorous with tireless work and endless creativity. This scientist researched anthrax and blood poisoning, published theories about germs and their application in medicine, about fermentation, and about puerperal fever.
At the age of 59, Louis Pasteur published research on yellow fever and succeeded in creating a vaccine against anthrax. Later, he studied swine erysipelas and developed a vaccine against this disease. July 1885 was a very important milestone in medical history when he successfully used a vaccine against rabies in humans.

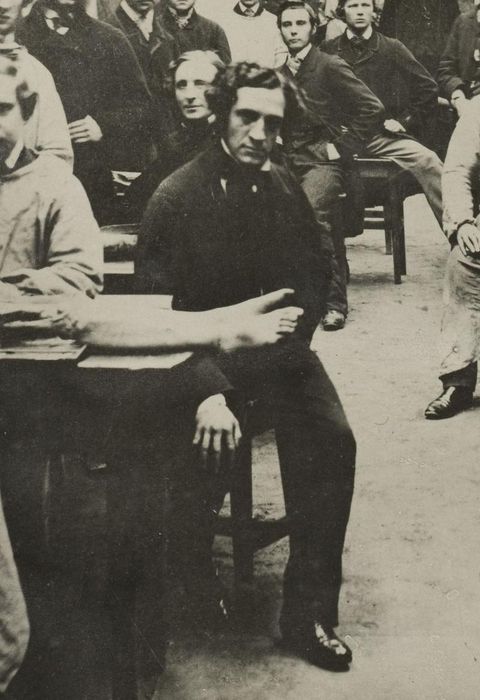
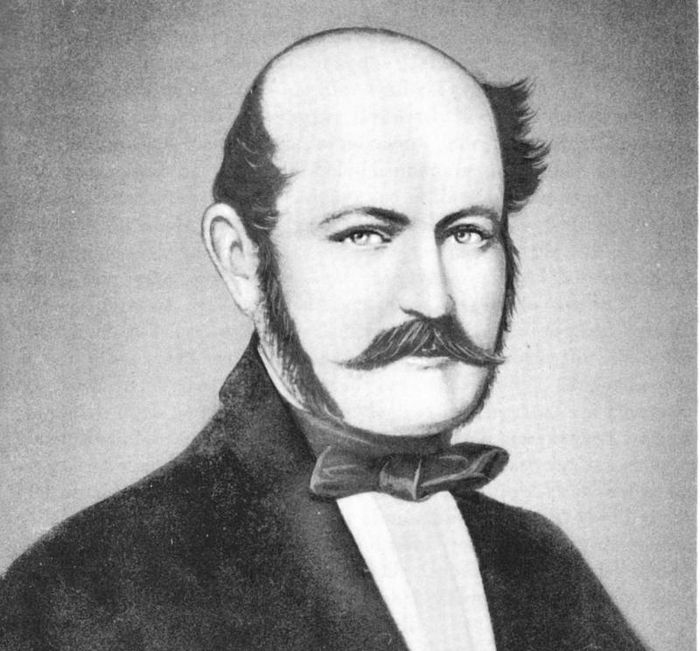
5. Physician Ignaz Semmelweis - Savior of Mothers
Ignaz Philipp Semmelweis was a Hungarian obstetrician. He asserted that puerperal fever was caused by infection. And he proved that the high mortality rate of mothers was due to doctors not washing their hands in Calcium Chloride solution before assisting with childbirth.
In 1861, he published a treatise on the cause, concept, and prevention of puerperal fever very clearly. In Hungary, the Semmelweis Museum was established. Semmelweis Hospital. In Austria, the Semmelweis Maternity Hospital was established and he was recognized in the world of medicine as the pioneer of the theory of antisepsis and hospital infection theory.
In 1847, he discovered that the incidence of puerperal fever could be greatly reduced by implementing handwashing standards in obstetric hospitals. Puerperal fever was common in hospitals in the mid-19th century, with a mortality rate of 10% - 35%. Semmelweis proposed handwashing with 'lemon water disinfected with chlorine' in 1847 in the position of chairman of the First Obstetric Department at the Vienna General Hospital, where the doctor's ward had a threefold death rate compared to that of the midwife's ward. In 1851, Semmelweis returned to Hungary, where his theory was accepted in 1857.
6. Dr. Elizabeth Blackwell - First Female Obstetrics Professor
Elizabeth Blackwell was born in Bristol (England), and her family immigrated to the United States in Cincinnati, Ohio. Since childhood, with a compassionate heart, she always wanted to learn more about the medical field to understand common illnesses better to help those around her. Blackwell was the first woman to receive a medical degree in North America (1849), furthermore, she graduated at the top of her class.
This had never happened in the history of medicine up to that time. In 1869, Elizabeth Blackwell helped organize the National Health Society in London (England) in activities such as free medical examinations and treatments for the poor, as well as establishing a medical school for women in London (London School of Medicine for Women). By 1875, she was appointed as the first female obstetrics professor at the London Children's Medical School.


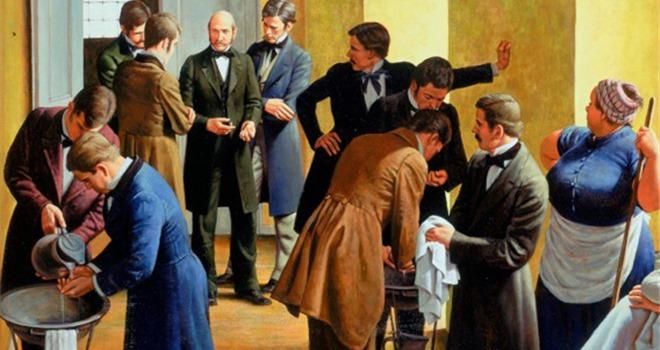
7. Dr. Joseph Lister - Father of Antiseptic Medicine
In 1861, Joseph Lister was appointed as a surgical physician at the Royal Infirmary in Glasgow. Here, he observed that 45% - 50% of patients died from wound infections. Joseph Lister, based on Louis Pasteur's theory, believed that infections were caused by microorganisms, and he used Carbolic Acid (phenol) for disinfecting surgical instruments and cleaning wounds.
As a result, the mortality rate in his surgeries significantly decreased due to this antiseptic. This led to a full recognition of the role of antiseptics in controlling infectious diseases. This was a significant historical milestone and one of the earliest efforts to control and mitigate surgical infections. In the early 19th century, surgical procedures became common in hospitals worldwide. However, due to a lack of awareness about surgical practices, the postoperative infection rate was often very high. To disinfect surgical instruments and clean wounds, British surgeon Joseph Lister experimented with carbolic acid.


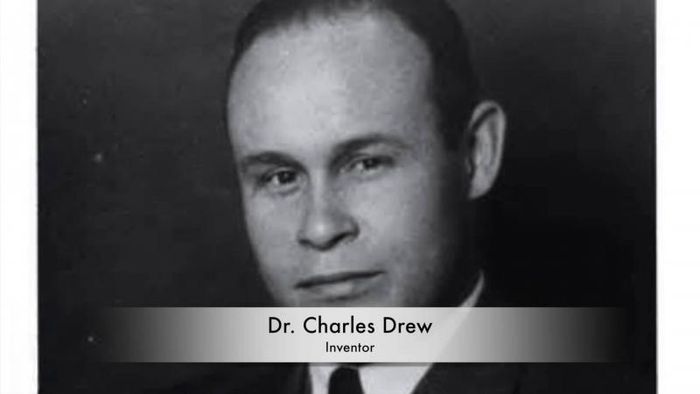
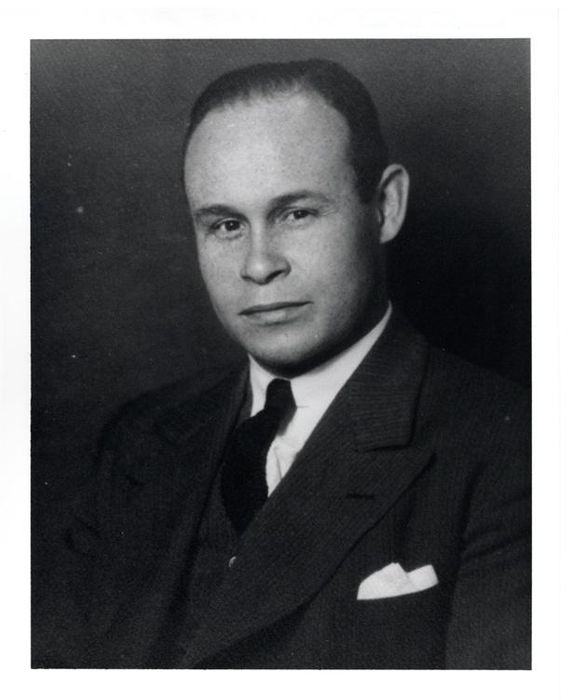
8. Dr. Charles Drew - Discoverer of Blood Plasma Separation and Preservation
Charles Drew, an African American physician, discovered the method to separate and preserve blood plasma. This breakthrough laid the foundation for establishing blood banks, which played a crucial role during World War II (1939 - 1945). He pioneered the creation of the first blood banks, saving thousands during the greatest loss in history.
At a time when millions of soldiers were dying on battlefields across Europe, Dr. Charles R. Drew's invention saved countless lives. Drew realized that separating and freezing the constituent parts of blood would allow it to be safely reconstituted later. This technique led to the development of blood banks.
Drew was born on June 3, 1904, in Washington, DC. Charles Drew excelled in academics and athletics, furthering his postgraduate studies at Amherst College in Massachusetts. He also was an honor student at McGill University Medical School in Montreal, where he specialized in physiology.
Charles Drew researched blood plasma and transfusions in New York City, where he became a medical scientist—the first African American to do so at Columbia University. There, he made discoveries related to blood preservation. By separating loose red blood cells from near-solid plasma and freezing them separately, he found that blood could be preserved and reconstituted the next day.
9. Dr. Frederick Banting - Discovery of Insulin Hormone
Frederick Banting, a Canadian physicist and physiologist, discovered the insulin hormone for treating diabetes. Born in 1891 in Alliston, Ontario, Banting studied at the University of Toronto. In 1915, he joined the medical corps and became a commanding officer. After World War I, he interned in London, Ontario, Canada.
From 1921 to 1922, he worked at the University of Toronto in the laboratory of Scottish physiologist John Macleod and Canadian colleague Charles Best. Banting discovered insulin, and in 1923, he was awarded the Nobel Prize in Physiology or Medicine with Macleod. The research team consisted of four members, with Banting and Best sharing half the prize, and Macleod and chemist James Bertramcllip (who helped purify insulin) sharing the other half. In 1923, the university established a medical research department, appointing Banting as its head. In 1934, he was knighted by the British royal family, marking the pinnacle of his career.
In 1921, Dr. Frederick Banting and medical student Charles H. Best were credited with discovering insulin hormone in extracts from a dog's pancreas. They injected insulin into a dog and found it reduced blood sugar levels from high to normal. They later refined their experiments, extracting and filtering the pancreas attached to a dog, isolating a substance called “isletin.” They then developed insulin for human use with the assistance of Canadian chemist James B. Collip and Scottish physiologist JJR Macleod. In 1923, he was awarded the Nobel Prize in Medicine for that groundbreaking discovery. Banting died in 1941 at the age of 50 due to a plane crash en route from Canada to war-torn England.

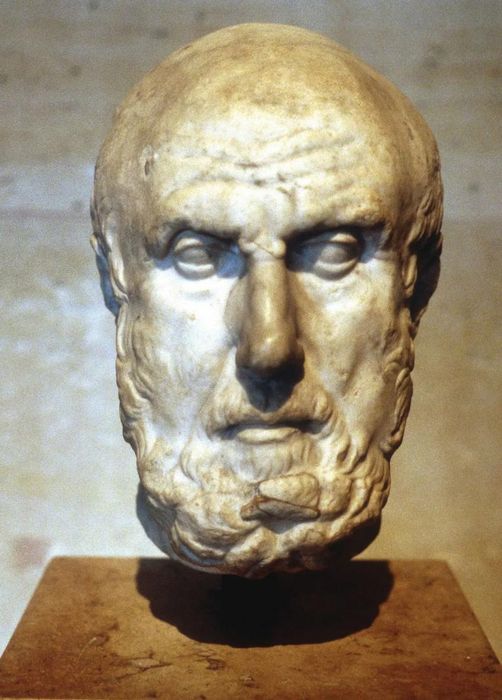
10. Dr. Henry Gray - Pioneering Anatomy
Dr. Henry Gray, an English anatomist, authored Gray’s Anatomy, laying the groundwork for the field of anatomy. At just 25, he was elected Fellow of the Royal Society and appointed surgeon-anatomist at St. George’s Hospital (England).
In 1861, he was the primary candidate for assistant surgeon, but tragically succumbed to smallpox while caring for a boy and passed away at the age of 34. Gray was born in Belgravia, London in 1827 and spent most of his life in London. In 1842, he enrolled as a student at St. George's Hospital, London, where he was known for his meticulous and methodical approach to anatomy, performing dissections slowly but meticulously, earning him the reputation of being the most methodical worker and anatomist of his time.
While still a student, Henry Gray won the Royal College of Surgeons University Prize in 1848 for an essay titled 'The Origin, Connection, and Distribution of the Nerves of the Human Eye and Their Appendages, Illustrated by Comparative Dissections of the Eye in Other Vertebrate Animals,' for which he received the Astley Cooper Prize of three hundred guineas for his dissertation 'On the Structure and Use of the Spleen.'
In 1858, Gray published the first edition of his anatomy book, comprising 750 pages and containing 363 illustrations. He was fortunate to have the assistance of his friend Henry Vandyke Carter, a skilled illustrator and former demonstrator of anatomy at St. George’s Hospital. Carter executed the drawings from which the engravings were made. The excellence of Carter's illustrations contributed significantly to the initial success of the book. This edition was dedicated to Sir Benjamin Collins Brodie, Bart, FRS, DCL. Gray held successive appointments as Demonstrator of Anatomy, Curator, and Lecturer on Anatomy at St. George’s Hospital, and in 1861 was a candidate for the position of Assistant Surgeon.