1. What Are Uterine Fibroids?
Uterine fibroids, also known as uterine leiomyomas, are benign tumors formed from the smooth muscle layer of the uterus. Contrary to common misconception, this is not a form of cancer. Uterine fibroids are the most common benign tumors in gynecology, occurring in 70% of women aged 30-45. However, there is a recent trend of fibroids appearing at younger ages. They are rarely seen after menopause. Approximately 25% of white women and 50% of black women have fibroids that develop symptoms.
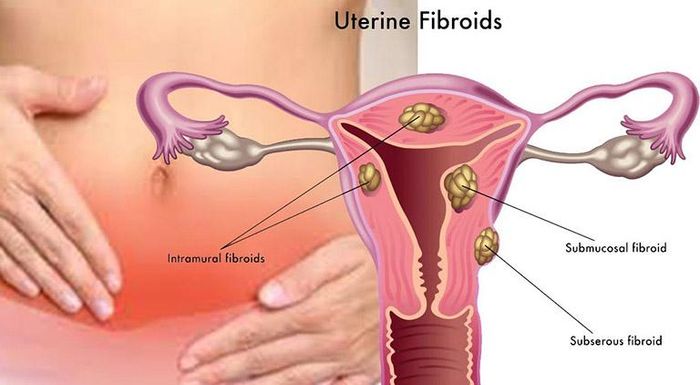
Most uterine fibroids are:
- Subserosal (outer layer of the uterine wall)
- Intramural (within the uterine wall)
- Submucosal (beneath the inner lining)
In some cases, fibroids may be located in the broad ligament, fallopian tubes, cervix, etc.
Fibroids are elastic, separate from the uterine wall, with sizes ranging from 1mm to 50mm. In each patient, the size and number of fibroids vary. Even though fibroids may be smaller than 50mm, they can weigh tens of kilograms. This can cause pain, bleeding, and in severe cases, infertility in women.

2. Symptoms of Uterine Fibroids
Most uterine fibroids are benign, hence they may not exhibit clinical symptoms. Only about 30-50% of patients have symptoms. Symptoms depend on the size and location of the fibroids, as well as whether the patient is pregnant or not.
Typically, uterine fibroids present with the following symptoms:
- Lower abdominal pain: Fibroids rarely cause pain, but patients may experience discomfort when the fibroid exceeds 50mm and compresses the ureter, bladder, rectum, and sometimes obstructs the bowel. The pain is usually dull and may become severe. Pain occurs when the fibroid becomes infected, degenerates, twists, or the uterus contracts to expel the fibroid.
- Abnormal vaginal bleeding (menorrhagia, metrorrhagia): This is a hallmark sign of this condition. When affected by uterine fibroids, patients often experience increased vaginal bleeding, prolonged menstrual cycles, clotted menstrual blood, or mixed with fragments of endometrial tissue. The blood is usually dark.
- Excessive foul-smelling vaginal discharge: Individuals with uterine fibroids often secrete abnormal amounts of foul-smelling vaginal discharge.
- Frequent urination: Large fibroids compress the bladder, causing the patient to feel the urge to urinate frequently.
- Pallor, fatigue, dizziness upon posture change, weight loss: Fibroids may compress blood vessels, increase venous pressure, and cause rupture of blood vessels. Bleeding causes anemia, reducing oxygen transport to the body, leading to fatigue, dizziness, and weight loss.
When experiencing any of the above abnormal symptoms, patients should not self-medicate at home but should seek medical attention promptly. Delaying treatment can lead to various dangerous complications, the most serious of which is infertility.


3. Risk Factors for Uterine Fibroids
Uterine fibroids are benign tumors. They occur due to sudden increases in hormones, especially estrogen. The rise in estrogen levels stimulates cells in the uterine wall to divide excessively and develop into fibroids. This explains why uterine fibroids are often found in women of childbearing age, when estrogen activity is high. Particularly during pregnancy, estrogen levels can peak. After menopause, hormonal activity decreases, making fibroids very rare.
However, if fibroids increase in size after menopause, there is a possibility of them transitioning to malignant tumors. However, this occurrence is extremely rare, with only about 0.2% chance of fibroids becoming cancerous.
In addition to hormonal activity, other factors contributing to this condition include:
- Genetic factors
- Inflammation of the cervix and uterus
- Being overweight or obese
Currently, scientists are still researching to accurately determine the causes of the increasing trend of uterine fibroids in younger women. Therefore, women aged 15-50, should undergo regular check-ups, including uterine fibroid ultrasound scans, to detect abnormalities early and follow appropriate treatment and monitoring methods.

4. How to Treat Uterine Fibroids?
Not all patients with uterine fibroids require treatment. In some cases, doctors may advise patients to monitor the fibroids for a period. For small uncomplicated fibroids, patients only need ultrasound scans and regular check-ups every 3 months, and most fibroids will shrink after menopause.
When fibroids grow in size accompanied by severe symptoms affecting quality of life, doctors may recommend one of the following methods:
- Medical treatment: using estrogen and progesterone inhibitors, injection therapy to necrotize fibroid nodules
- Surgical treatment: fibroid removal surgery, subtotal or total hysterectomy
Currently, newer methods may alleviate symptoms, but the duration of symptom reduction and the effectiveness of these methods in preserving reproductive function are not yet evaluated. These treatment options include:
- High-intensity focused ultrasound
- Cryotherapy
- Radiofrequency ablation of fibroids
- Convergent ultrasound surgery combined with MRI-guided focused ultrasound
- Uterine artery embolization
Therefore, hysterectomy remains the most definitive and effective treatment method. However, hysterectomy leads to loss of fertility. Hysterectomy can be performed via open surgery, laparoscopic or robotic-assisted abdominal surgery, or vaginal hysterectomy. Hence, patients should carefully consider and consult with their doctors before undergoing treatment methods.


5. Complications of Uterine Fibroids
U xơ tử cung gây những biến chứng khác nhau tùy thuộc vào tình trạng tồn tại có thai hay không có thai.
Đối với phụ nữ chưa có thai, những biến chứng của u xơ tử cung có thể là:
- Chậm có thai hoặc vô sinh: người bệnh mắc u xơ tử cung có thể không có thai trong một thời gian dài dù không sử dụng bất kì biện pháp tránh thai nào
- Nhiễm khuẩn: tình trạng xuất tiết khí hư có mủ, mùi khó chịu, chảy máu âm đạo bất thường kết hợp việc bệnh nhân vệ sinh vùng kín kém sẽ dễ gây nhiễm khuẩn đường âm đạo. Nghiêm trọng hơn còn làm tăng nguy cơ hóa ác thành ung thư cổ tử cung và ung thư tử cung
Đối với phụ nữ có thai, u xơ tử cung sẽ gây ra một số biến chứng sau đây:
- Sảy thai: khi mắc u xơ tử cung, cơ thành tử cung đàn hồi kém, dẫn tới rối loạn co bóp và tăng nguy cơ sảy thai, sinh non. Tỉ lệ sảy thai ở thai phụ mắc u xơ tử cung cao hơn những người bình thường khi mang thai
- Rau bong non: việc hình thành khối u ở dưới rau thai sẽ chèn ép khiến rau thai bị bong tróc ra. Điều này gây thiếu dinh dưỡng và oxy cung cấp cho thai nhi, ảnh hưởng nghiêm trọng tới tính mạng của người mẹ và thai nhi
- Cản trở đường sinh tự nhiên của thai nhi: việc kích thước khối u phát triển, nhất là ở eo và cổ tử cung, sẽ gây cản trở đường ra tự nhiên của thai nhi. Thai phụ phải sinh mổ
- Xuất huyết ồ ạt khi sổ thai: do khối u làm ảnh hưởng tới niêm mạc tử cung nên sau khi sổ thai, cơ tử cung khó co lại để cầm máu được
Chính vì những biến chứng nghiêm trọng của căn bệnh này, phụ nữ khi mang thai nên đi siêu âm định kì và thăm khám đều đặn để kịp thời phát hiện những dấu hiệu bất thường. Từ đó có phương pháp điều trị và kế hoạch sinh hợp lý (sinh tự nhiên hay sinh mổ).


