Scabies is a widespread condition that affects individuals of all ages, ethnicities, and economic statuses across the globe. It is not caused by poor hygiene. The scabies mite, scientifically known as Sarcoptes scabiei, is a parasitic organism that lives on the skin and causes scabies. The mite has eight legs and can only be seen under a microscope. Female mites burrow into the epidermis (the outermost layer of the skin) to make their home, search for food, and lay eggs. They rarely penetrate the stratum corneum, the outermost layer of the epidermis. If you suspect you have scabies, follow the steps below to identify or diagnose the condition, as well as learn about treatment and future prevention methods.
Steps
Watch for signs of scabies

Itching sensation. Scabies presents with several symptoms, with the most common and earliest sign being a persistent itching sensation. This is a skin reaction to the female scabies mite, its eggs, and its waste products.
- The itching tends to worsen at night and can lead to sleeplessness for the affected individual.

Notice the rash symptoms. Along with itching, you may experience a rash, which is also an allergic reaction of the body to mites. The rash usually appears as red, swollen, round bumps. Another key feature is that mites tend to settle in specific areas of the skin.
- In adults, common places for the rash to appear are the hands, particularly the skin between the fingers, wrist creases, elbows, knees, buttocks, waist, genitals, around the nipples, armpits, shoulder blades, and chest.
- For children, mites prefer to nest in areas such as the scalp, face, neck, palms, and soles.

Locate the mite nests. When dealing with scabies, you might occasionally spot tiny burrows in the skin, which are winding, slightly raised, grayish-white or skin-colored lines. These mite nests typically range from one centimeter in length or longer.
- However, it is often difficult to find their nests, as there are usually only 10-15 mites present during a scabies outbreak.

Pay attention to skin lesions. Scabies causes intense itching and sometimes leads to skin ulcers, which carry a high risk of infection, a common complication of scabies. These ulcers are often infected by bacteria like Staphylococcus aureus or group A streptococcus, which can then spread across the skin.
- These bacteria can also cause kidney inflammation and even blood poisoning, a life-threatening condition.
- To avoid this, you should refrain from scratching and handle your skin gently. If you can't resist, consider wearing cotton gloves or using band-aids on your fingertips to prevent further damage. Remember to trim your nails.
- Signs of infection include redness, swelling, increased pain, or ulcer drainage, such as pus or fluid. Seek medical attention if you suspect the rash has become infected. The doctor may prescribe topical antibiotics or oral medication to treat the infection.

Flaky skin. This is another sign of scabies, specifically Norwegian scabies, which is a more severe form of the disease. It is characterized by small blisters accompanied by thick, scaly skin spreading across the body. Norwegian scabies primarily affects individuals with weakened immune systems. A weakened immune response allows mites to reproduce freely, with some outbreaks involving up to two million mites.
- A compromised immune system can also reduce the severity of symptoms like itching and rashes, or even eliminate them entirely.
- Older adults with weakened immune systems, or those with HIV/AIDS, lymphoma, or leukemia, are more likely to develop Norwegian scabies. You may also be at risk if you've undergone organ transplants or suffer from conditions that numb or impair sensation, such as spinal cord injury, paralysis, or neurological disorders.
Scabies Diagnosis

Clinical Evaluation. If you suspect you have scabies, it's essential to see a doctor promptly for a clinical diagnosis. The doctor diagnoses scabies by examining the rash and mite nests.
- They use a small needle to scrape a tiny piece of skin, which is then observed under a microscope to detect mites, eggs, or their waste products.
- It’s important to note that you may still have scabies even if no mites, eggs, or waste are found under the microscope, as only about 10-15 mites are present in a single outbreak across the body.

Ink Test. A doctor may use an ink test to identify mite nests. Ink is applied to the affected area, and then a cotton pad soaked in alcohol is wiped over the ink. If mite nests are present, the ink will remain in the winding tracks and appear as dark, squiggly lines.

Excluding Other Skin Conditions. There are many other skin conditions that could be mistaken for scabies. The presence of mite nests is the key distinguishing feature of scabies, as no other skin condition has such nests. Your doctor will help rule out other possibilities to ensure your condition is scabies.
- Scabies is sometimes confused with insect bites or flea stings.
- Impetigo, which is also highly contagious, can resemble scabies. The red spots from impetigo primarily appear on the face, around the nose and mouth.
- Scabies can also be confused with eczema, a chronic skin inflammation. In eczema, the body’s allergic reaction manifests as a red, raised rash. Those with eczema can also develop scabies, making the condition worse.
- Folliculitis, an infection around hair follicles, can also be mistaken for scabies. It results in white-headed bumps surrounded by redness, located around or near hair follicles.
- Psoriasis shares some similarities with scabies. It’s a chronic inflammatory skin disease characterized by excessive skin cell growth, leading to thick, silvery scales and numerous itchy, dry, red patches.
Scabies Treatment

Using Permethrin. To treat scabies, you must eradicate all mites with a prescription medication. Currently, no over-the-counter medication is effective for scabies treatment. Doctors typically prescribe a 5% permethrin cream to eliminate the mites and their eggs. The application involves spreading it from the neck down to the entire body, followed by a bath after 8-14 hours.
- Reapply the cream after 7 days (one week). Possible side effects include itching or a sensation similar to pricking.
- Consult your doctor before treating scabies in infants and young children. Permethrin cream is safe for infants as young as one month, but most experts recommend applying it to the head and neck of babies and young children. However, avoid applying the cream to the child’s eyes and mouth.

Use of Crotamiton 10% Cream or Lotion. Crotamiton cream or lotion is another prescription medication for treating scabies. Apply it from the neck down to the entire body after a bath. A second dose is applied 24 hours after the first, followed by a bath after 48 hours. Repeat this two-dose regimen after 7-10 days.
- Crotamiton is considered safe when used as prescribed, but there have been reports of its ineffectiveness in treating scabies, meaning it may no longer be the most effective treatment or widely used.

Use of 1% Lindane Lotion. Lindane lotion, like other scabies treatments, is applied from the neck down to the entire body, followed by a bath after 8-12 hours for adults, and after 6 hours for children. Reapply the medication after 7 days. Lindane should not be used in children under 2 years old, pregnant women, breastfeeding mothers, or individuals with weakened immune systems.
- The medication can be neurotoxic, meaning it can harm the brain and other parts of the nervous system. Lindane should only be prescribed for individuals who have not responded to other treatments or cannot tolerate less risky alternatives.

Use of Ivermectin. Ivermectin is an oral treatment for scabies. Studies show that it is both safe and effective, although it has not been approved by the U.S. Food and Drug Administration (FDA) for scabies treatment. Ivermectin is prescribed as a single dose of 200 mcg/kg, taken with water on an empty stomach.
- Another dose may be taken after 7-10 days. Ivermectin is considered only for individuals who have not responded to FDA-approved topical treatments or cannot tolerate them.
- A common side effect of ivermectin is an increased heart rate.

Treating Skin Irritation. The symptoms and skin damage from scabies may take up to three weeks to heal, even if the mites have been completely eliminated. If skin damage persists during this time, you may need another treatment, as the previous one may not have been successful or the condition may have recurred. Cooling the skin is an effective way to relieve itching. You can do this by soaking in a cool bath or applying a cold compress to the affected areas.
- Adding oatmeal or baking soda to your bath can enhance skin soothing.
- Calamine lotion can also be used to treat mild skin irritation. The best options for itching relief include Sarna or Aveeno anti-itch creams. Avoid products with fragrances or dyes, as they can further irritate the skin.

Steroid Creams or Oral Antihistamines. Both steroid creams and oral antihistamines can help treat itching caused by scabies, which is essentially an allergic reaction to the mites, their eggs, and their waste. Steroids are potent anti-itch and anti-inflammatory agents, with examples like betamethasone and triamcinolone being commonly used.
- Since this is an allergic reaction, over-the-counter antihistamines can also be used to alleviate itching, such as Diphenhydramine, Dorotec, Loratadine, and Telfast BD. These are especially helpful at night for easier sleep. Diphenhydramine also has a mild sedative effect. Prescription antihistamines, like Atarax, are also available.
- Hydrocortisone 1% cream, available over-the-counter, can also be quite effective in relieving itching.
Prevention of Scabies

Be Cautious to Avoid Exposure. The most common way scabies spreads is through direct skin-to-skin contact with an infected person, with prolonged contact increasing the risk. The disease can also spread through indirect contact with items such as bedding, pillows, clothing, and furniture, although the risk is lower. Mites can survive for 48-72 hours outside the human body. In adults, scabies often spreads through sexual activity.
- Crowded living conditions are a common cause of scabies outbreaks, so places like prisons, military camps, daycare centers, nursing homes, and schools are frequent sources of infection. Scabies cannot be spread through animals.
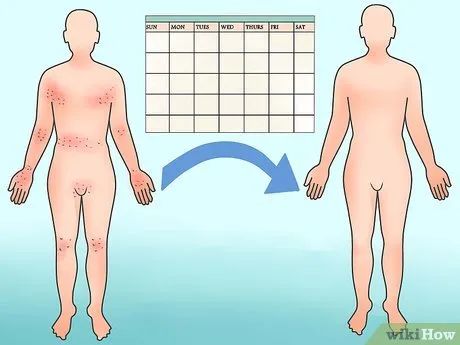
Understanding the Incubation Period. After initial scabies exposure, symptoms and signs typically take 2-6 weeks to develop. Keep in mind that an infected person can still transmit scabies even if no symptoms are present.
- For those who have been previously infected, symptoms tend to develop much faster, within 1-4 days.

Identifying High-Risk Groups. Certain groups of people are more likely to spread scabies to others, including children, mothers with young children, sexually active adults, residents of nursing homes, maternity centers, and extended care facilities.
- The increased risk of transmission in these groups comes from frequent skin-to-skin contact.

Household Hygiene and Sterilization. Preventing reinfection often requires cleaning and sterilizing the home alongside treatment. These measures should be followed for all household members who have close contact with the infected person, including their partner.
- On the first day of treatment, wash all clothes, bed linens, and towels used in the past 3 days in hot water and dry them on the highest heat setting, or have them dry-cleaned. If washing or dry-cleaning is not possible, place these items in a sealed plastic bag for at least 7 days. Mites can only survive 48-72 hours off the skin.
- Also, on the first day, vacuum floors and furniture. Dispose of or empty the vacuum bag, and clean the dust container. If the dust container cannot be removed, use a damp paper towel to wipe the mites inside.
- Do not treat pets for scabies. The mites causing scabies cannot live on animals, and animals cannot spread scabies to humans.
- There is no need to use insecticide sprays to eliminate scabies mites from the environment.
Advice
- Children and adults can resume normal activities such as attending school or work once treatment has begun.
Warnings
- Seek medical attention if the rash does not improve within 2-3 weeks, worsens, recurs after treatment, or appears to be infected (with increased redness, swelling, or pus).
